Translate this page into:
Evaluation of awareness and knowledge regarding mandibular reconstruction in interns and postgraduates: A cross-sectional study
*Corresponding author: Kashif Mohammed, Department of Oral and Maxillofacial Surgery, VSPM’s Dental College and Research Center, Nagpur, Maharashtra, India. kashifmp3112@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mohammed K, khandaitkar S, Shenoi R. Evaluation of awareness and knowledge regarding mandibular reconstruction in interns and postgraduates: A cross-sectional study. J Adv Dental Pract Res 2022;1:64-7.
Abstract
Objectives:
Many conditions such as malignancy, osteomyelitis, osteonecrosis, or osteoradionecrosis affect oral cavity particularly the jaw by impairing the bone formation and resorption process. Eradication of these conditions may sometimes require resection of whole of jaw bone or a part of it. Reconstruction or rehabilitation of the lost part is necessary for higher quality of life. Hence, it is important to bring this topic to limelight and evaluate the level of knowledge. Furthermore, it is important to assess awareness present among interns and postgraduates (PGs) for the reconstruction techniques. The overarching aim of this study was to conduct a survey to evaluate the awareness and knowledge regarding different mandibular reconstruction among interns and PGs.
Materials and Methods:
An online questionnaire-based study using Google forms was carried out among interns and PGs of VSPM’s dental college and research center. General characteristics, designation, reconstruction techniques, goals and criteria for reconstruction, grafts, and classification of defects were assessed.
Results:
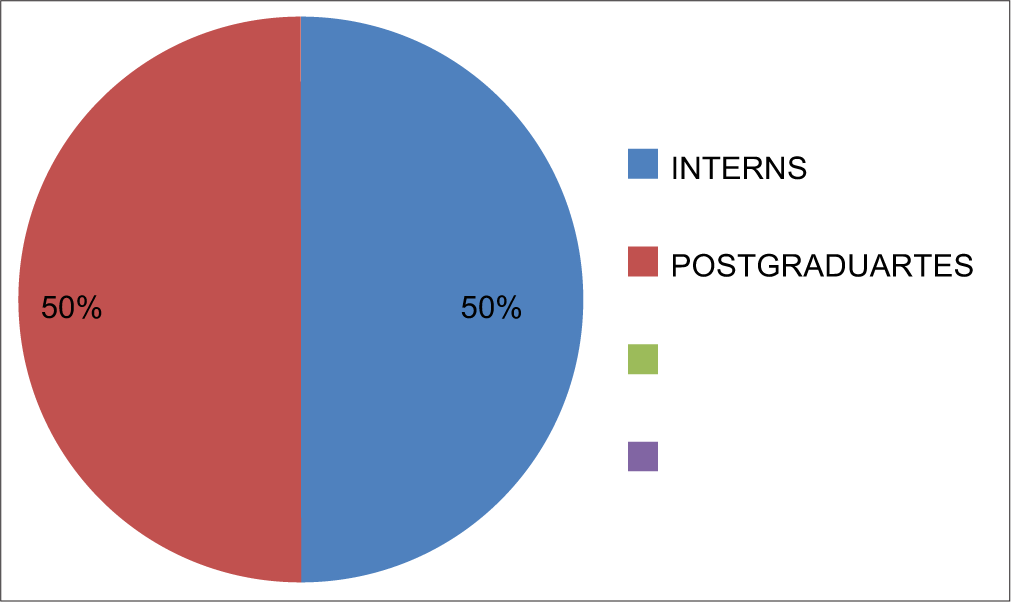
A total of 100 participants participated in the survey. About 50% among them were interns and 50% were PG students. About 92% of PG participants were aware about the different mandibular techniques, while among the interns only 88% were aware.
Conclusion:
A significant difference existed in responses collected from interns and postgraduate. PG students were more aware about the reconstruction and rehabilitation options. Further, upgradement of technologies in this field can improve quality of life of cancer patients and dentist can help to provide it. Knowledge and attitude toward rehabilitation can improve the promptness of delivery of health services.
Keywords
Rehabilitation
Vascularized flaps
Non-vascularized flaps
INTRODUCTION
In India, oral cancer exists as a major public health issue affecting the oral cavity.[1] Oral cavity consists of tongue, lips, buccal mucosa, and jaws. The prevalence of oral cancer accounts for 20/100,000 population. Similarly, other conditions affecting jaws include osteomyelitis due to infection, osteonecrosis as a result of radiation in the head and neck region, medication related osteonecrosis, certain benign, and malignant tumors like ameloblastoma. Mainstay of treatment in these conditions is mainly surgery including resection of complete jaw or a part of it, which leads to explicit esthetic and functional disfigurement.
Resection of mandibular jaw bone is called mandibulectomy. Removal of jaw bone lowers the quality of life of individuals. Several problems such as eating speech defects, decreased jaw opening, appearance, esthetics, and psychological issues emerge after mandibulectomy. To overcome all these issues, several reconstruction techniques have been tried over century. Mandibular reconstruction has evolved significantly over the years and continues as newer technologies and biocompatible materials are being introduced.[2]
Reconstruction involves a multidisciplinary approach and compressive reconstructive strategies involving restoration of function and esthetics.[2]
Dentoalveolar segments, soft-tissue envelope, and buttresses of jaw bone are important for achieving optimal height and dimensions.[2] Type of defect helps in selecting an appropriate approach for reconstruction. Improvement of facial contours, establishment of continuity, function, arch form, and width are some of the major goals and criteria involved with reconstruction.[2] Another important factor governing reconstruction is timing of it.
Reconstruction plates and screws, various non-vascularized and vascularized free grafts, and pectoralis major myocutaneous flap have been tried in the past. Recent advances include transport disc distraction osteogenesis (TDDO), endoprosthesis, and tissue engineering.[2] Virtual planning and 3D printing modeling have the potential to increase mandibular reconstruction accuracy and reduce operation time.[3] Even though newer technologies are available, vascularized free flaps provide the best results. They are considered gold standard of reconstruction procedures.[3] The most feared outcome of mandibular reconstruction is graft failure.[4]
Even though there is a concomitant rise in cancer cases in India, awareness about rehabilitation after the surgery or resection has not reached every individual. Dentist can play a crucial role in creating awareness about rehabilitation and provide for a higher quality of life for their patients. Hence, I aimed to study the awareness and perception of interns and postgraduate (PG) students mandibular reconstruction and rehabilitation and to bring to the limelight the recent advances of the field.
Objectives
This study aims to evaluate level of knowledge about various mandibular reconstruction techniques among interns and postgraduates and amount of awareness that exists about this topic in them.
MATERIALS AND METHODS
A cross-sectional study was carried out in VSPM’s DENTAL COLLEGE AND RESEARCH CENTER among interns and PGs. The Institutional Ethics Committee approved the study approval number IEC/VSPMDCRC/75/2022. A total of 100 participants participated in the survey. About 50% participants were interns and the rest 50% were postgraduates. A self-administered questionnaire in the form of Google forms was circulated to the participants. The link was closed after 100 responses were collected. Data collected were compiled in excel sheet and analyzed using IMB SPSS 2020 software. Chi-square test was used to compare the variables. The questionnaire was used to collect demographic data, designation, various techniques of reconstruction, classification of defects, and recent advances.
RESULTS
A total of 100 responses were collected. Mean age of participants was 23.79 years [Table 1]. About 68% of the participants were female and rest 32% were male [Table 2 and Figure 1].
| Descriptive Statistics | |||||
|---|---|---|---|---|---|
| N | Minimum | Maximum | Mean | Std. Deviation | |
| Age | 100 | 22 | 28 | 23.79 | 1.217 |
| Gender | Frequency | Percent |
|---|---|---|
| Valid | ||
| Female | 68 | 68.0 |
| Male | 32 | 32.0 |
| Total | 100 | 100.0 |
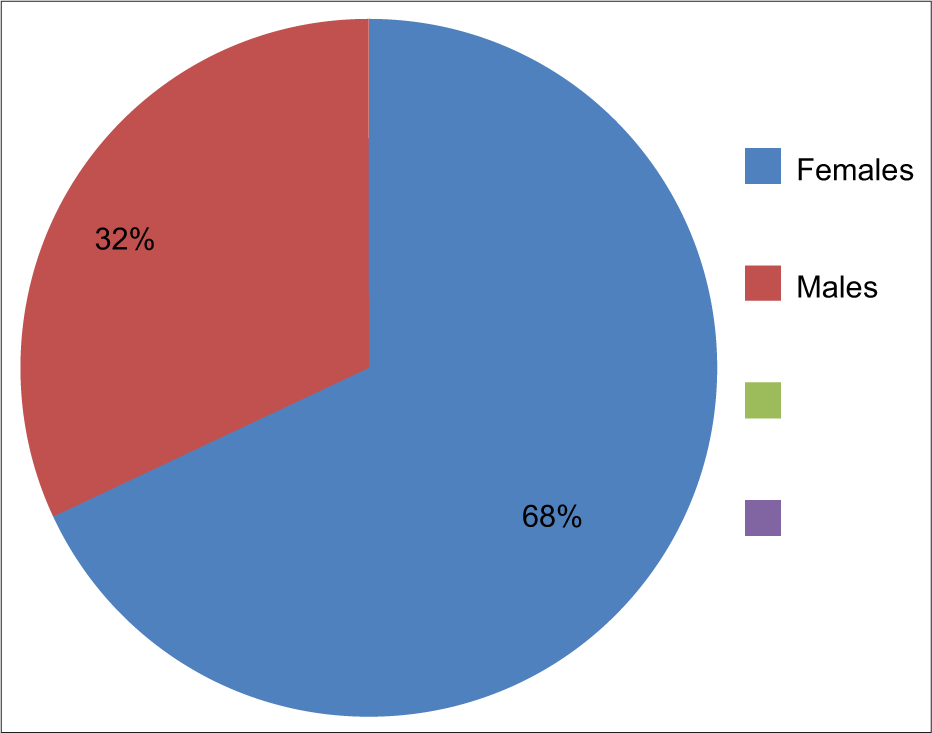
- Gender.
A descriptive analysis of the result is shown below [Table 3]. About 88% of intern participants were aware about mandibular reconstruction techniques and 92% of the participants from postgraduate group were aware [Table 3 and Figure 2]. About 74% of the PG students gave correct answers about ideal treatment for mandibular defects, while 23% of them were not aware. Among the interns group, 52% of the participants perception about ideal treatment was incorrect. Only 48% of them could correctly answer about it. About 78% of the participants of PG group would bethink of comprehensive reconstructive strategies, while 28% were unable to recollect. Similarly, 66% of interns could correctly identify the strategies and 34% were unable to do so. About 70% of PGs and 56% of the interns were well acquainted with the goals and criteria of mandibular reconstruction techniques, while 30% of PGs and 44% of interns were not well versed. About 58% of PGs knew about JEWER classification of mandibular defects and 42% of them were not well versed with the classification. While 60% of the individuals had no idea about the classification, only 40% could correctly answer. Only 44% PGs were able to correctly identify the reconstructive options that rest 56% failed to do so. Among interns, only 28% were aware that rest 72% did not have enough knowledge about various reconstructive options. About 76% PGs correctly identified the most predominantly used flap for consular reconstruction in children and adolescents and rest 24% were unable to correctly guess the flap, while 56% of the interns could correctly guess the flap, 44% of them failed. Only 34% of PG students could correctly answer about most efficient reconstruction option for mandibular body defects that remaining 66% of them were unaware about the method. Similarly, 74% intern participants were unaware, only 26% of them could respond to the question correctly. About 60% of PGs were acquainted with the factors essential for autogenous bone replacement, while 40% were not. Among intern group, a majority of 70% of participants were not aware about essential factors for determination of bone replacement. Only 30% of them could correctly answer. About 64% of PGs responded correctly about the newer recent advancements made in this field, 36% of them were unaware, while 68% of the intern participants were unaware and only 32% of them could respond correctly.
| Designation | Total | P-value | ||
|---|---|---|---|---|
| Intern | Postgraduate | |||
| 1. Are you aware of mandibular reconstruction techniques? | ||||
| No | 6 (12) | 4 (8) | 10 | |
| Yes | 44 (88) | 46 (92) | 90 | 0.505 |
| Total | 50 (100) | 50 (100) | 100 | |
| 2. Ideal treatment for mandibular defects include | ||||
| Incorrect | 26 (52) | 13 (26) | 39 | |
| Correct | 24 (48) | 37 (74) | 61 | 0.008* |
| Total | 50 (100) | 50 (100) | 100 | |
| 3. Comprehensive reconstructive strategies require | ||||
| Incorrect | 17 (34) | 11 (22) | 28 | |
| Correct | 33 (66) | 39 (78) | 72 | 0.181 |
| Total | 50 (100) | 50 (100) | 100 | |
| 4. Goals and criteria of mandibular reconstruction techniques include | ||||
| Incorrect | 22 (44) | 15 (30) | 37 | |
| Correct | 28 (56) | 35 (70) | 63 | 0.147 |
| Total | 50 (100) | 50 (100) | 100 | |
| 5. Jewer classified mandibular defects into | ||||
| Incorrect | 30 (60) | 21 (42) | 51 | |
| Correct | 20 (40) | 29 (58) | 49 | 0.044* |
| Total | 50 (100) | 50 (100) | 100 | |
| 6. Reconstructive options for mandibular reconstruction are | ||||
| Incorrect | 36 (72) | 28 (56) | 64 | |
| Correct | 14 (28) | 22 (44) | 36 | 0.023* |
| Total | 50 (100) | 50 (100) | 100 | |
| 7. Which graft is used predominantly for consular reconstruction in children and adolescent | ||||
| Incorrect | 22 (44) | 12 (24) | 34 | |
| Correct | 28 (56) | 38 (76) | 66 | 0.035* |
| Total | 50 (100) | 50 (100) | 100 | |
| 8. Most efficient for defects of the mandibular body for reconstruction of continuity defects is | ||||
| Incorrect | 37 (74) | 33 (66) | 70 | |
| Correct | 13 (26) | 17 (34) | 30 | 0.383 |
| Total | 50 (100) | 50 (100) | 100 | |
| 9. Techniques for autogenous bone replacement is determined by the following factors | ||||
| Incorrect | 35 (70) | 20 (40) | 55 | |
| Correct | 15 (30) | 30 (60) | 45 | 0.008* |
| Total | 50 (100) | 50 (100) | 100 | |
| 10. Recent advances in mandibular reconstruction | ||||
| Incorrect | 34 (68) | 18 (36) | 52 | |
| Correct | 16 (32) | 32 (64) | 48 | 0.000** |
| Total | 50 (100) | 50 (100) | 100 | |
- Designation.
DISCUSSION
Oromandibular reconstruction has drastically changed over the decades. Various modalities are now available to choose from according to the case. We as health-care providers also need to continuously keep upgrading our knowledge as per the need of our patients and society. TDDO, distraction osteogenesis, and medical modeling[3] are the newer advancements in the field of reconstruction and future clinicians should be aware in details about these new tools. The most important complications in mandible reconstruction include reconstruction plate exposure, free flap failure, and serious cardiopulmonary problems.[4] To overcome these problems, it is necessary to be well versed and well acquainted with these techniques.
A significant difference existed among the responses collected from PGs and interns. PG students had higher level of perception that interns about the ideal treatment option which can be provided for patients requiring mandibular reconstruction. P = 0.008 was found to be significant. Similarly, a significant difference in knowledge and awareness was observed (P = 0.0008) while assessing factors which need to be determined during autogenous bone replacement.
Ideal treatment plan can be prescribed only when one has a knowledge about the defects requiring reconstruction and rehabilitation. A significant value was obtained (P = 0.04) during assessment of knowledge about classification of defects. PG students currently pursuing their degree course were more aware about the newer reconstruction techniques available than interns. Interns lacked the comprehension regarding newer procedures and advanced rehabilitation methods. All other parameters were not found to be significant, which may be due to limited number of participants and less area and experience barrier present in the study. Thus, there is need to increase exposure of the interns group to this topic so that when they set up their private clinical practice or join any institution, they can provide better life to their patients and higher standard of living.
Limitations of the study were that it was conducted amongst a very small population and conducted in a single institution and hence results cannot be extrapolated to other colleges or professionals. Furthermore, the questionnaire was self-administered and distributed in the same institution so there is a chance of informal discussions among respondents and it may be the reason for variation in the responses.
CONCLUSION
Amount of knowledge and awareness about mandibular reconstruction is present but scarce among dental graduates and PGs. Although the level of knowledge and awareness came out to be significant in the other group, there is need to create more awareness and thus acquaint the dental students with this topic.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Oral cancer diagnosis and perspectives in India. Sens Int. 2020;1:100046.
- [CrossRef] [PubMed] [Google Scholar]
- Mandibular reconstruction: Overview. J Maxillofac Oral Surg. 2016;15:425-41.
- [CrossRef] [PubMed] [Google Scholar]
- Virtual Planning and 3D printing modeling for mandibular reconstruction with fibula free flap. Med Oral Patol Oral Cir Bucal. 2018;23:e359-66.
- [CrossRef] [PubMed] [Google Scholar]
- Oral rehabilitation of segmental mandibulectomy patient with osseointegrated dental implant. Contemp Clin Dent. 2014;5:209-12.
- [CrossRef] [PubMed] [Google Scholar]