Translate this page into:
Comparative analysis of stress distribution in implant attachment versus cantilever prostheses
*Corresponding author: Hojatollah Yousefimanesh, Department of Periodontology, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran. yousefimanesh-h@ajums.ac.ir
-
Received: ,
Accepted: ,
How to cite this article: Neghab S, Kouchehbaghi K, Salehizeinabadi M, Yousefimanesh H. Comparative analysis of stress distribution in implant attachment versus cantilever prostheses. J Adv Dental Pract Res. 2024;3:40-51. doi: 10.25259/JADPR_33_2024
Abstract
Objectives:
Dental implants are essential for replacing missing teeth, but anatomical constraints can result in implant sites being distant from adjacent teeth. Cantilever implant prosthetics offer an alternative solution by bridging this gap. This study compares the efficacy of cantilever implant prosthetics with conventional implant placement directly adjacent to teeth.
Material and Methods:
Using cone beam computed tomography, 3-D models were constructed to accurately represent the anatomy of teeth 4, 5, and the surrounding jawbone. Two models were examined: (1) a pontic with a cantilever implant abutment and (2) a pontic connected to both an implant and a tooth abutment. Simulation testing applied forces of 100 Newton in vertical, horizontal, and 45° directions to mimic functional loads on anterior teeth. Analytical processes were conducted using specialized finite element analysis software.
Results:
In model 1, tension levels under a 100 N force at a 45° angle were 80.1 in the implant and 66.5 in the implant’s crown. In model 2, tensions decreased to 58.26 in the implant and 35.8 in the crown under the same conditions. Connecting the tooth to the implant significantly reduced the load on both components, indicating potential biomechanical benefits.
Conclusion:
The attachment of dental implants to adjacent teeth presents a suitable alternative for patients with challenging anatomical considerations.
Keywords
Implant
Finite element analysis
Cantilever
Implant stability
INTRODUCTION
Dental implants have revolutionized the restoration of complete and partial edentulism, significantly enhancing masticatory function, patient satisfaction, and overall quality of life compared to conventional prosthetics reliant on natural teeth.[1] In partial edentulism reconstruction, implant-supported bridges are often the preferred choice.[2] Implant-based restorations not only provide optimal support without relying on soft tissue and muscles but also stimulate bone, preserving its size and dimensions.[1] However, challenges such as limitations in implant placement, failures in osseointegration, alveolar bone deficiencies, patient reluctance towards ridge augmentation, and economic constraints persist, prompting consideration of combined implant and natural tooth approaches.[3,4]
The intense osseointegration between implants and bone introduces differences in displacement and movement patterns compared to natural teeth, potentially leading to complications such as implant component loosening and anomalies in stress distribution around implants.[4-8] Proposed solutions to minimize these complications include the use of non-rigid connectors and stress-absorbing elements in implants.[4,6] However, the debate between non-rigid connectors and rigid connections persists.[6]
Connecting implants to adjacent teeth is proposed in cases where noticeable lateral movement or conditions suggesting horizontal forces on the abutment tooth are present, offering options for final prosthesis design.[9] Cantilevers in fixed prosthetics pose challenges due to torque forces on the abutment, leading to common complications such as loss of cement and subsequent debonding or bone breakdown.[10]
Implants, being harder than natural teeth, are subject to greater force on the cement seal in implant abutments, making cantilevering implants less favorable compared to natural teeth and potentially leading to complications such as prosthesis failure.[11] Excessive cantilever forces can be mitigated by connecting implants to adjacent teeth.[10,12]
Although surgical success rates for implants exceed 98%, early loading failures can occur due to biomechanical factors, particularly with short implants or implants in soft bone.[13] Mechanical complications associated with implants include abutment screw loosening, prosthesis cement fracture, and biomechanical stress leading to marginal bone analysis or peri-implantitis.[13,14] Stress primarily enters the implant-bone interface due to the absence of a periodontal ligament in implants, impacting the marginal bone.[13,15]
Key principles for implant placement in fixed prostheses include eliminating cantilevers, avoiding three consecutive pontics, and considering specific locations for implant placement based on tooth absence.[16] Teeth exhibit greater physiological movement compared to implants, emphasizing the importance of careful consideration during treatment planning.[17]
In connecting implants to teeth, certain conditions must be met to reduce biomechanical stress and associated risks. Unilateral force should be avoided on a one-sided prosthesis, and connecting a rigid implant to an anterior tooth is possible when lateral forces are clinically acceptable. However, due to significant clinical mobility, connecting implants to a single anterior tooth is rare, necessitating an increase in the number of implants for stress reduction.[3] Stress distribution around dental implants is evaluated through methods such as finite element analysis (FEA), which simulates different clinical scenarios to predict stress patterns and optimize implant designs.[18] While FEA provides valuable insights, it is crucial to complement it with clinical evaluations.[19] FEA’s role in predicting stress patterns in clinical conditions has been demonstrated in several studies, highlighting its significance in dental research.[20-24] Understanding the bio-mechanical aspects of dental implants and their connection to natural teeth is crucial for optimizing treatment outcomes. The proposed study aims to compare stress distribution in the connection of an implant to a tooth versus a cantilever implant prosthesis using FEA.
MATERIAL AND METHODS
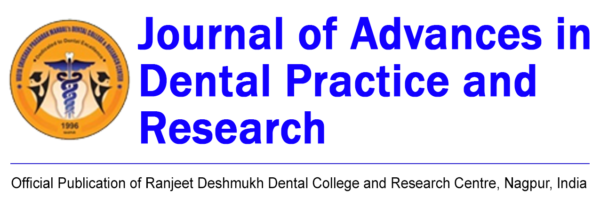
In this study, an accurate three-dimensional (3-D) lower jaw contour was initially created using cone beam computed tomography (NewTom Giano, Newtom, Imola, Italy) data from an actual patient in Materialise Mimics (Materialise, Leuven, Belgium) V10.01 software. The generated model in Standard Triangle Language (file format commonly used for 3D printing and computer-aided design) format was then transferred to rapid form and Geomagic Studio software. In these software packages, the created meshes were optimized, unnecessary points and regions were removed, and holes resulting from data transfer were repaired. The volume of information in the 3-D shape was reduced to facilitate the final analysis. Subsequently, the existing 3-D mesh was fitted to the surfaces, and a 3-D editable volume was prepared from the created surfaces [Figure 1].
- The necessary steps for modelling and using the scanned file of the jaw. CBCT: Cone-beam computed tomography, DICOM: Digital imaging and communications in medicine, PTC: Prototyping tool center, INP: Input file, STL: Standard tessellation language, PDL: Periodontal ligament, CT: Computed tomography.
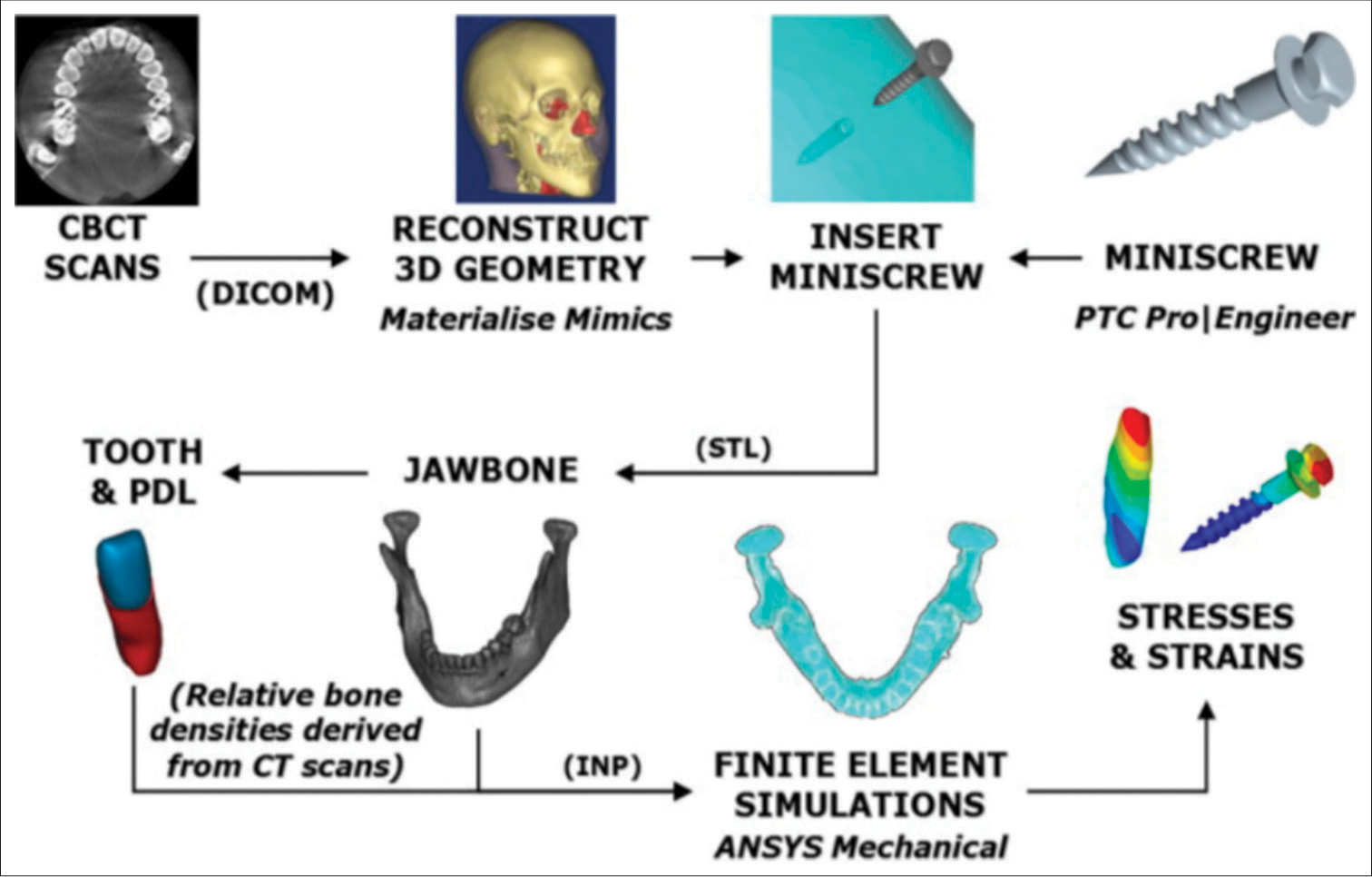
The output from Mimics software can be directly transferred to Abaqus [Figure 2]; however, it is non-editable. Due to the necessity of adding implants and modeling various scenarios of tooth, abutment, and implant connections, Rapid form software was utilized. The final file was then transferred to the powerful Abaqus software for FEA.
- Mimics software.
In this study, the implant (Biohoraizons Internal, Implant system Inc., Birmingham, Al, USA) with a length 12 mm and diameter 4 mm was initially drawn and created using the manufacturer’s catalog. Subsequently, the components of the jaw, including cortical and cancellous bone (obtained from Mimics software), and the crown from the actual tooth and implant, were assembled and assigned appropriate materials. After loading onto the implants and teeth, and establishing suitable boundary conditions for the upper jaw, and meshing the hole shape, the results were compared.
Evaluated modes
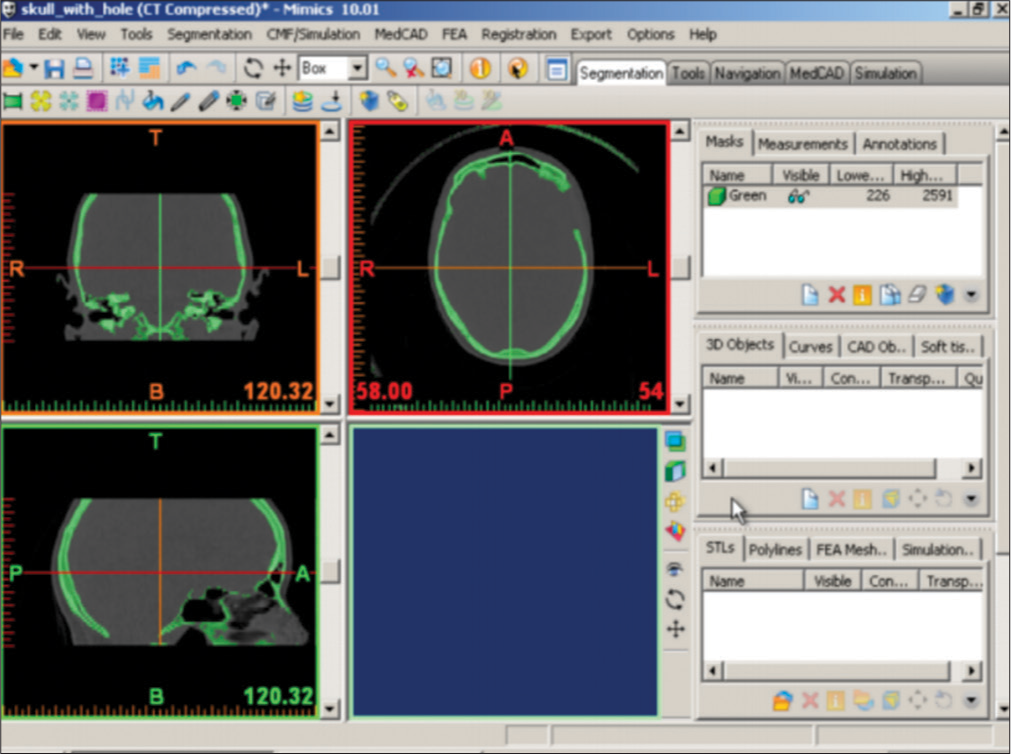
In this project, two models have been created and reviewed. The first mode is created by connecting three tooth veneers, as shown in Figure 3.
- First model created by connecting three tooth veneers.
However, in the second model, the fourth tooth is not connected to the fifth and sixth teeth, and this difference in the connection method will cause a difference in stress distribution [Figure 4].
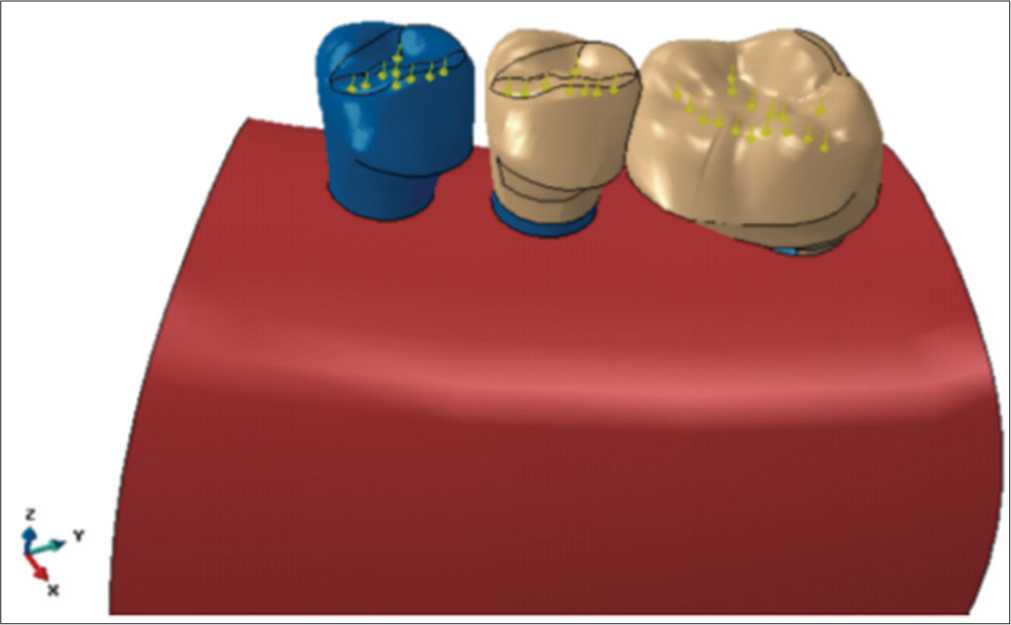
- Second model created by disconnecting the fourth tooth.
The mesh model generated in Abaqus software: After utilizing Geomagic software and creating surfaces from the mesh generated in Mimics software (by generating and editing surfaces, smoothing surfaces, optimizing meshes, removing noise, etc.), it is necessary to mesh the model as shown in Figure 5. The number of nodes and elements has been determined through trial and error to both ensure convergence of the problem solution and enable the representation of the original shape with appropriately dimensioned and angled elements (each comprising small components).
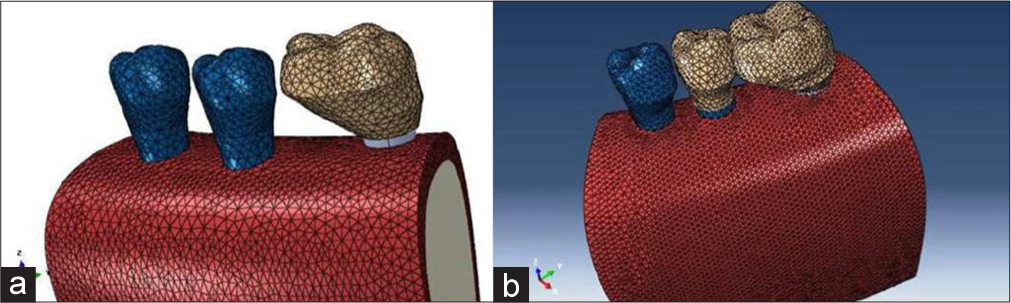
- Mesh applied to the: (a) first model and (b) second model.
Loading and application of forces
The applied force on each tooth was set to 100 Newtons, and its angle of application [Figure 6] was adjusted to model various loads on the crown, tooth, and implant. The angle was varied at 0, 15 +, and 45 + degrees, and the applied force was distributed at multiple points in a manner that prevented the concentration of stress at a single point.
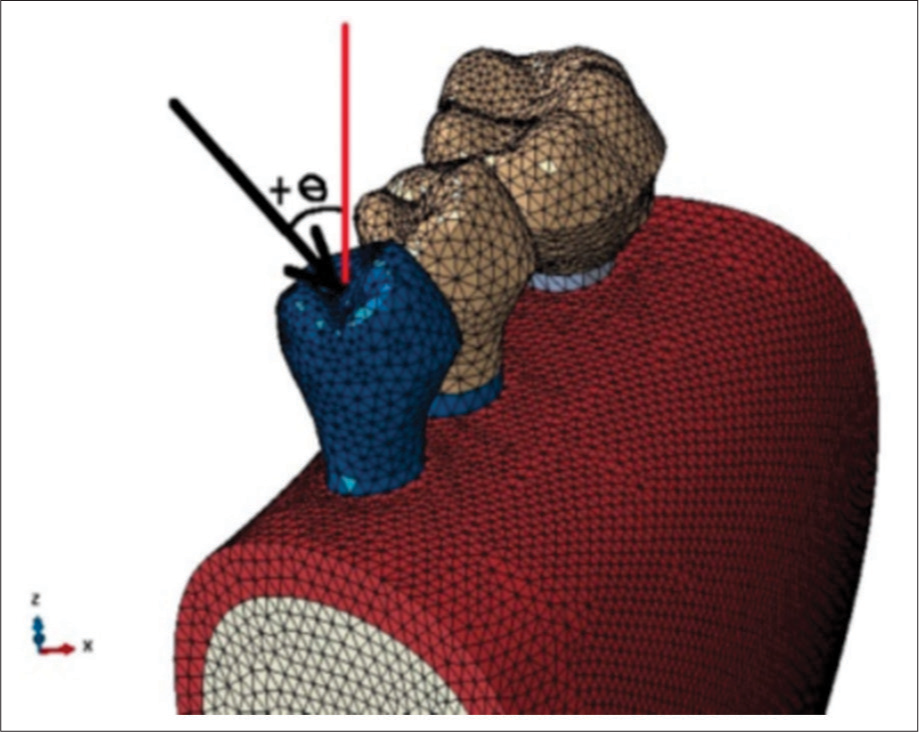
- Applying the force with the specific angulation. (+θ: the angle between the applied force and tooth long axis)
According to the figure, for the application of loads to the teeth, the total load is distributed among 20 points on each tooth in a way that each point in the loading condition with a 0° angle is required to withstand 5 Newtons of force. In the figure below, a view of the powerful Abaqus software, along with its modules is presented. The Part module is used for component construction. The implant model in this project was created using the dimensions from the manufacturer’s catalog. The Property menu is used for assigning appropriate materials to each component of the model. The Assembly menu is used for assembling various parts (jaw bones, implant, crow, and tooth). The Step menu is utilized for defining the type of problem, the Load menu is used for loading the problem, the Mesh menu is employed for meshing and element generation, the Job menu is for defining the problem-solving approach, and the Visualization menu is for observing the results. Considering that the simulation method was used in the research, there is no need to determine the sample size. To compare the two models, if the data in the two groups are normal, we use t-test and if they are not, we use Mann–Whitney test, which was done by the Statistical Package for the Social Sciences version 9 software.
RESULTS
The values of von Mises stress in the cortical and cancellous bone around the implant, crown structure, tooth 4, and tooth 5 subjected to a force of 100 Newtons in three directions, 0, 15, 45° relative to the crystal surface of model A and B are compared in Table 1 and shown in Figures 7-12.
| Direction Force (°) | Amount of stress (MPa) in model A | Amount of stress (MPa) in model B |
|---|---|---|
| Stress distribution in cortical bone | ||
| 0 | 19.3 | 36.6 |
| 15 | 32.2 | 15 |
| 45 | 53 | 30 |
| Stress distribution in cancellous bone | ||
| 0 | 3.6 | 2.72 |
| 15 | 3.67 | 3 |
| 45 | 2.97 | 3.14 |
| Stress distribution in the implant | ||
| 0 | 41.6 | 27.19 |
| 15 | 44.1 | 27.2 |
| 45 | 80.1 | 58.26 |
| Stress distribution in the implant’s crown | ||
| 0 | 56 | 33.3 |
| 15 | 58.1 | 34 |
| 45 | 66.5 | 35.8 |
| Stress distribution in tooth 4 | ||
| 0 | 15.4 | 15.4 |
| 15 | 26.5 | 27.7 |
| 45 | 60 | 60 |
| Stress distribution in tooth 5 | ||
| 0 | 19 | 36.6 |
| 15 | 30 | 36.9 |
| 45 | 69 | 70 |
MPa: Megapascal
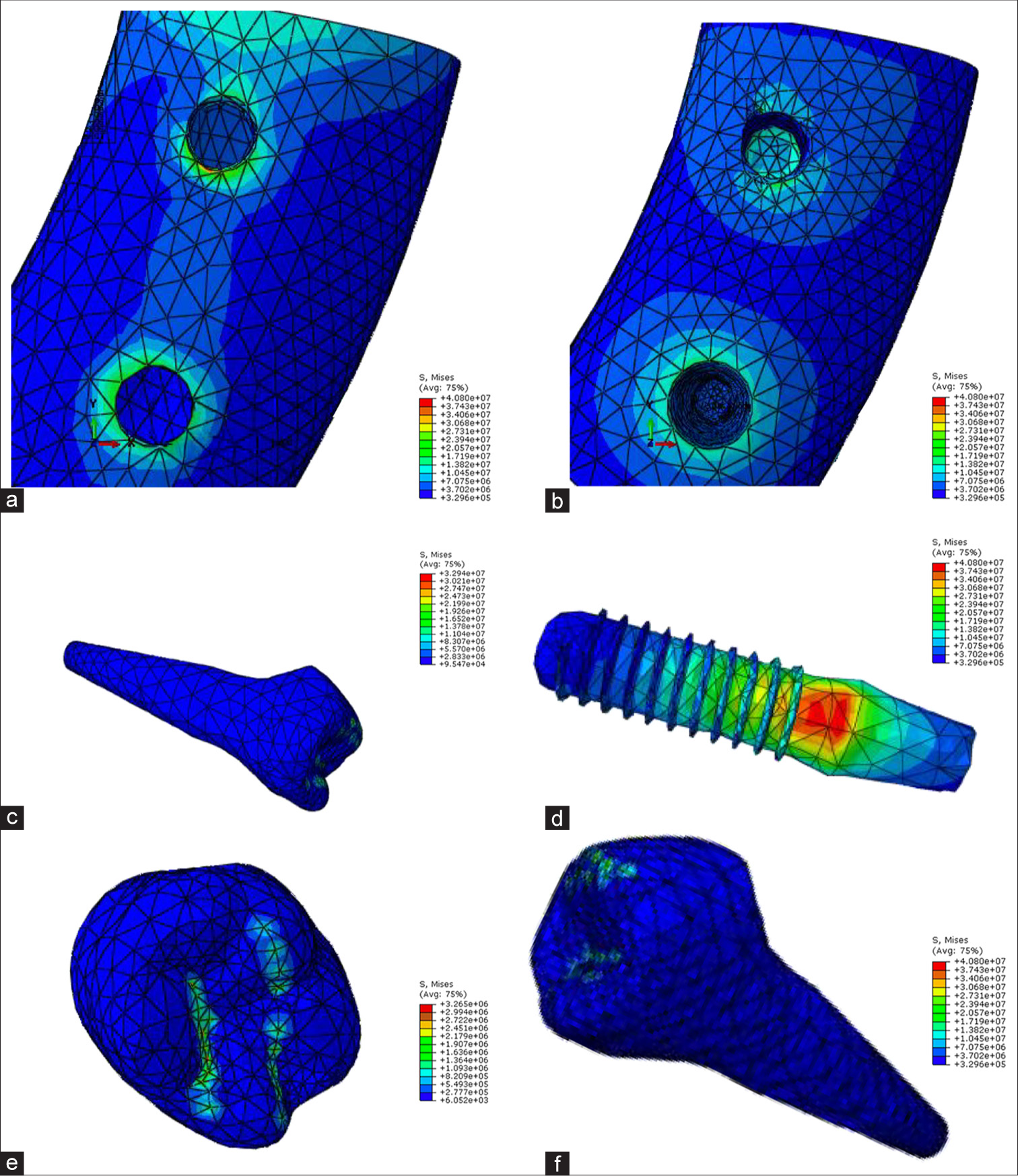
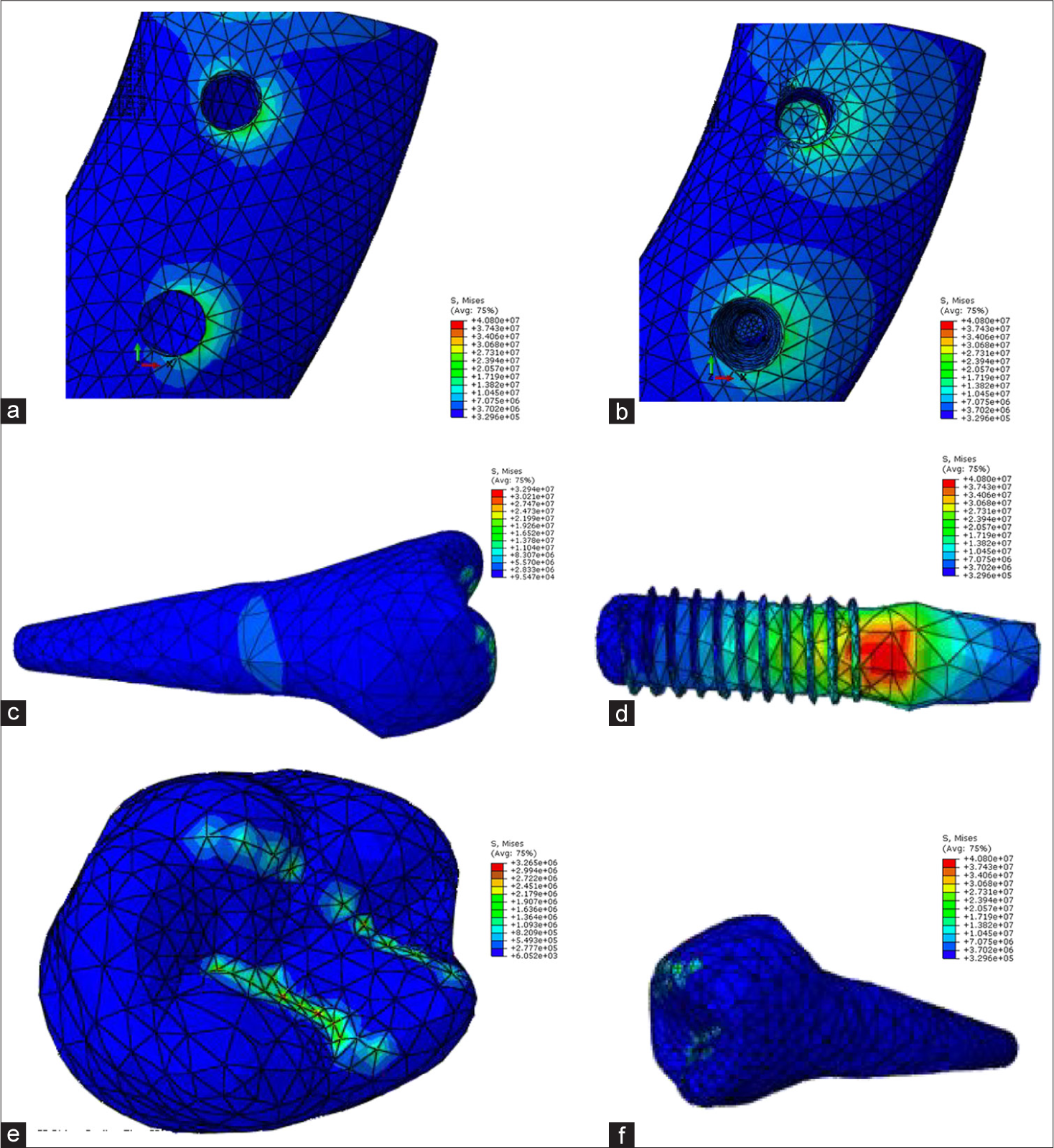
- Model A, force angle 0 (a) Cortical bone, (b) cancellous bone, (c) tooth 5, (d) implant, (e) crown, (f) tooth 4.
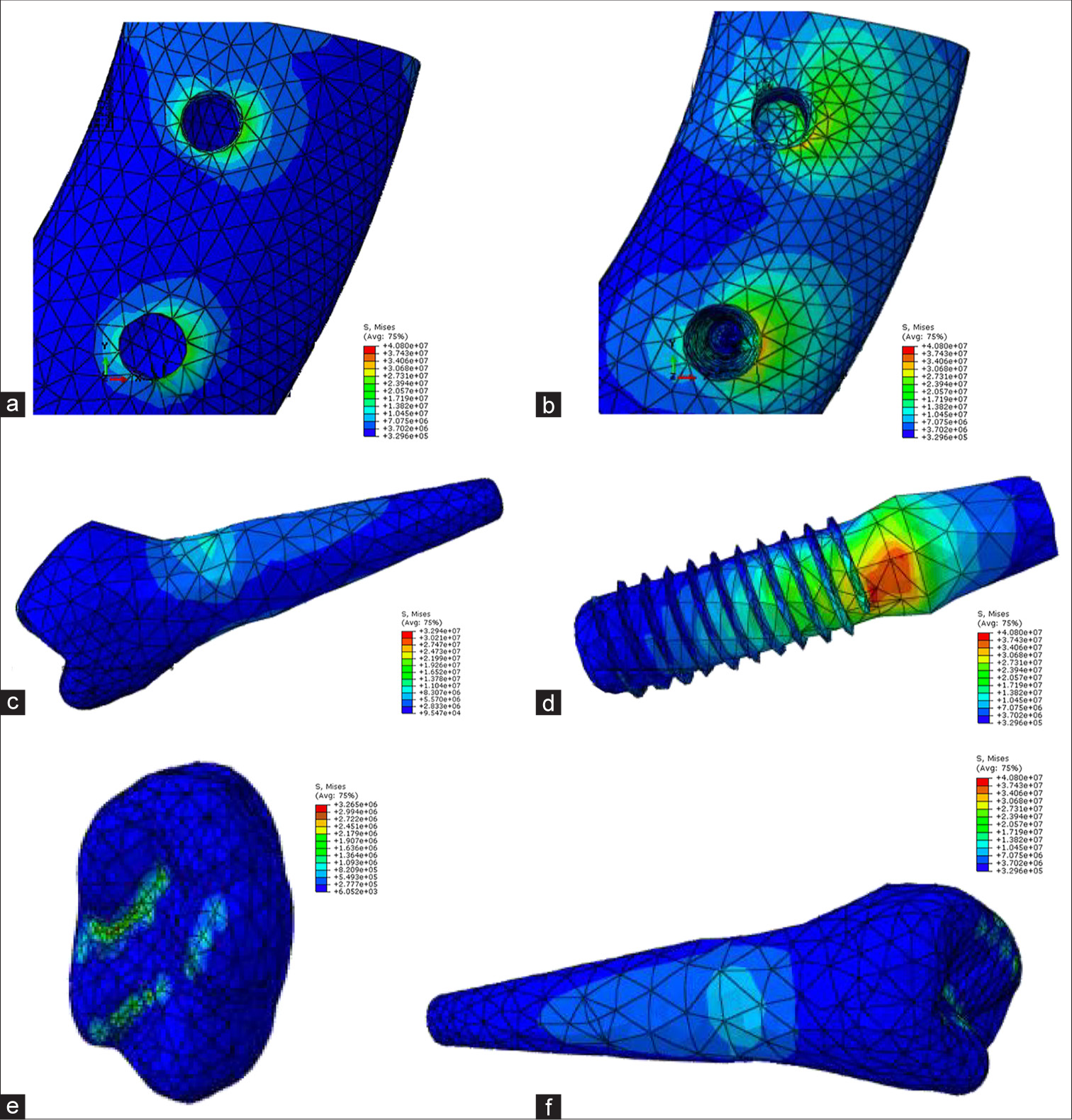
- Model A, force angle 15 (a) Cortical bone, (b) cancellous bone, (c) tooth 5, (d) implant, (e) crown, (f) tooth 4.
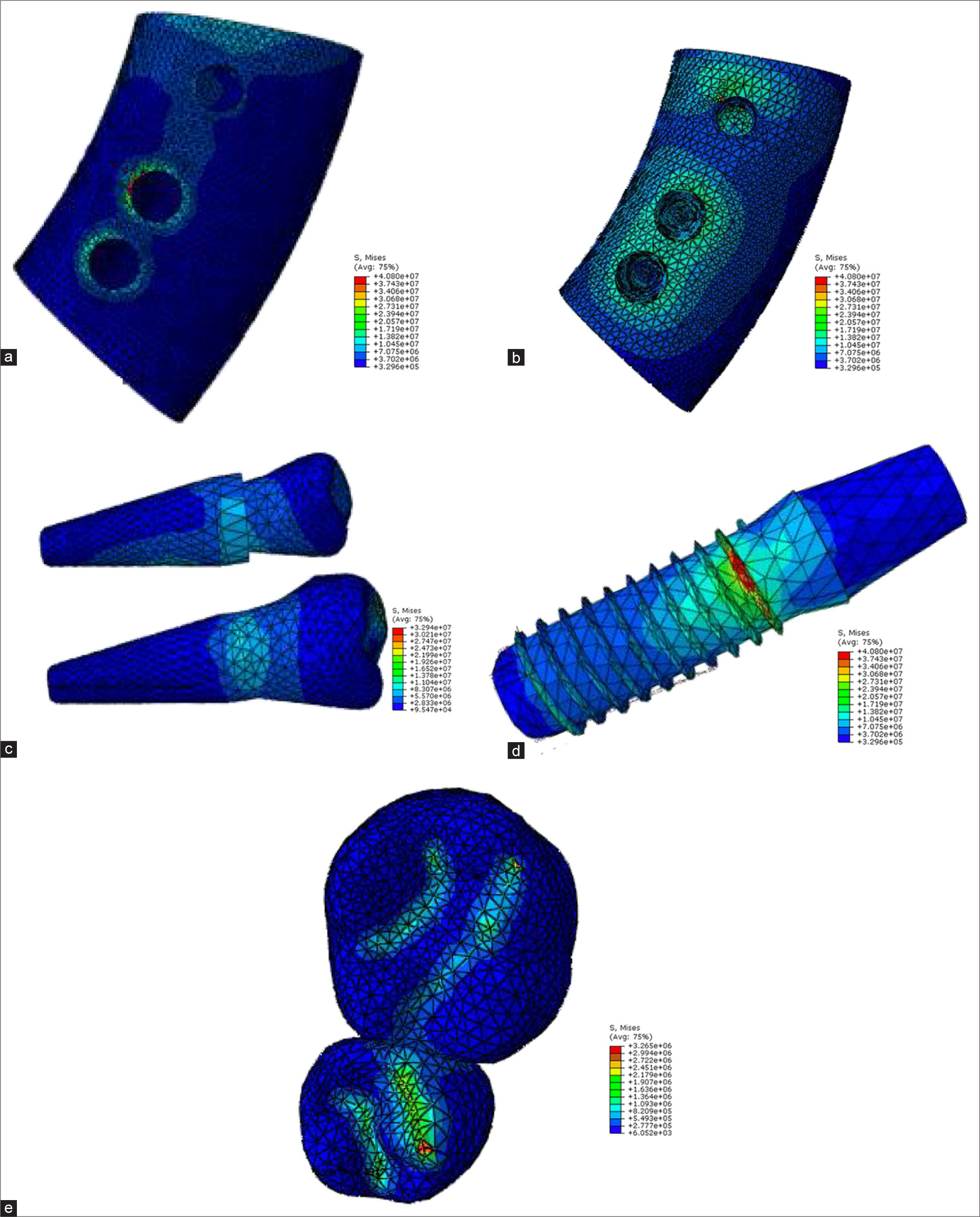
- Model A, force angle 45 (a) Cortical bone, (b) cancellous bone, (c) tooth 5, (d) implant, (e) crown, (f) tooth 4.
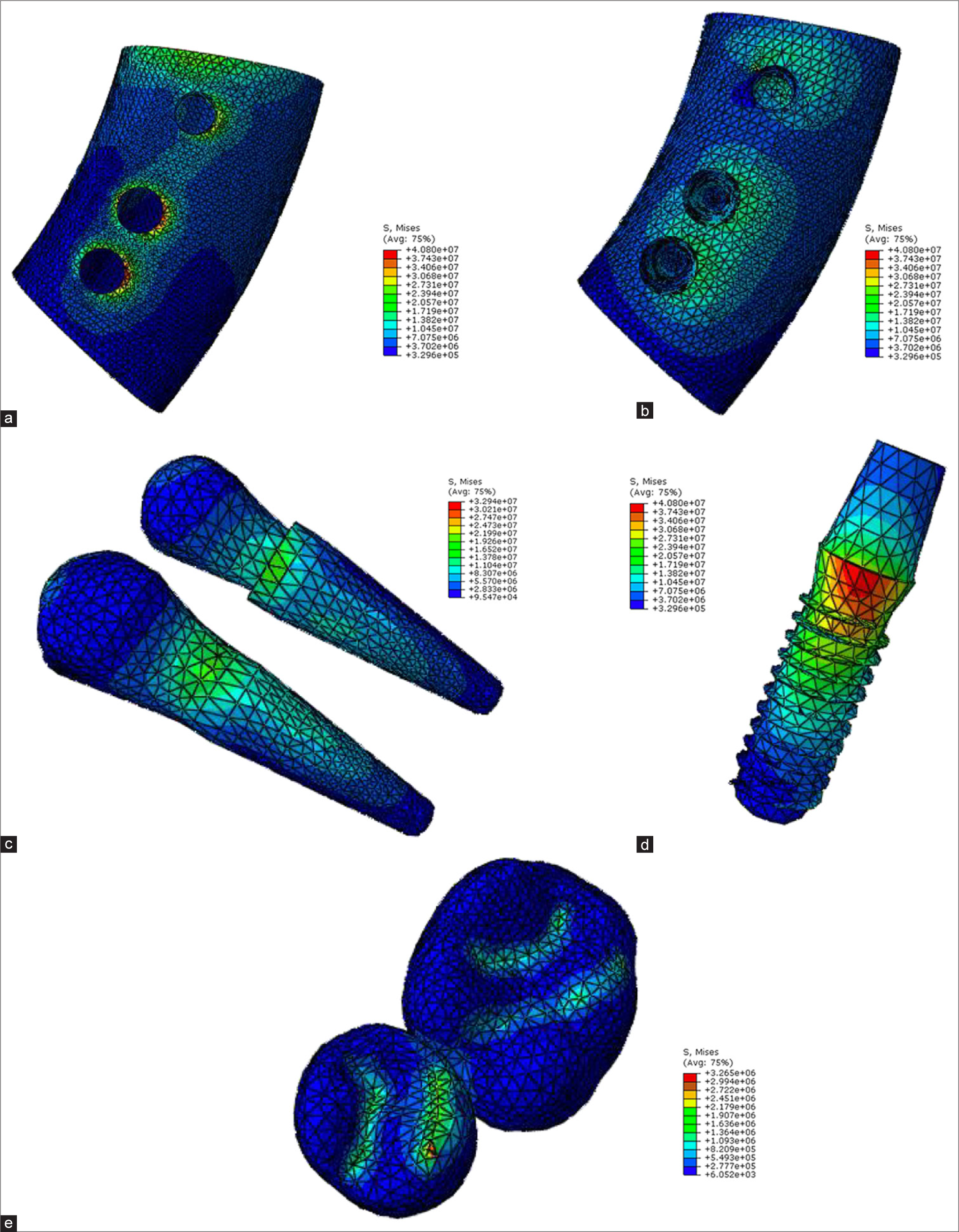
- Model B, force angle 0 (a) Cortical bone, (b) cancellous bone, (c) teeth 4 and 5, (d) implant, (e) crown.
- Model B, force angle 15 (a) Cortical bone, (b) cancellous bone, (c) teeth 4 and 5, (d) implant, (e) crown.
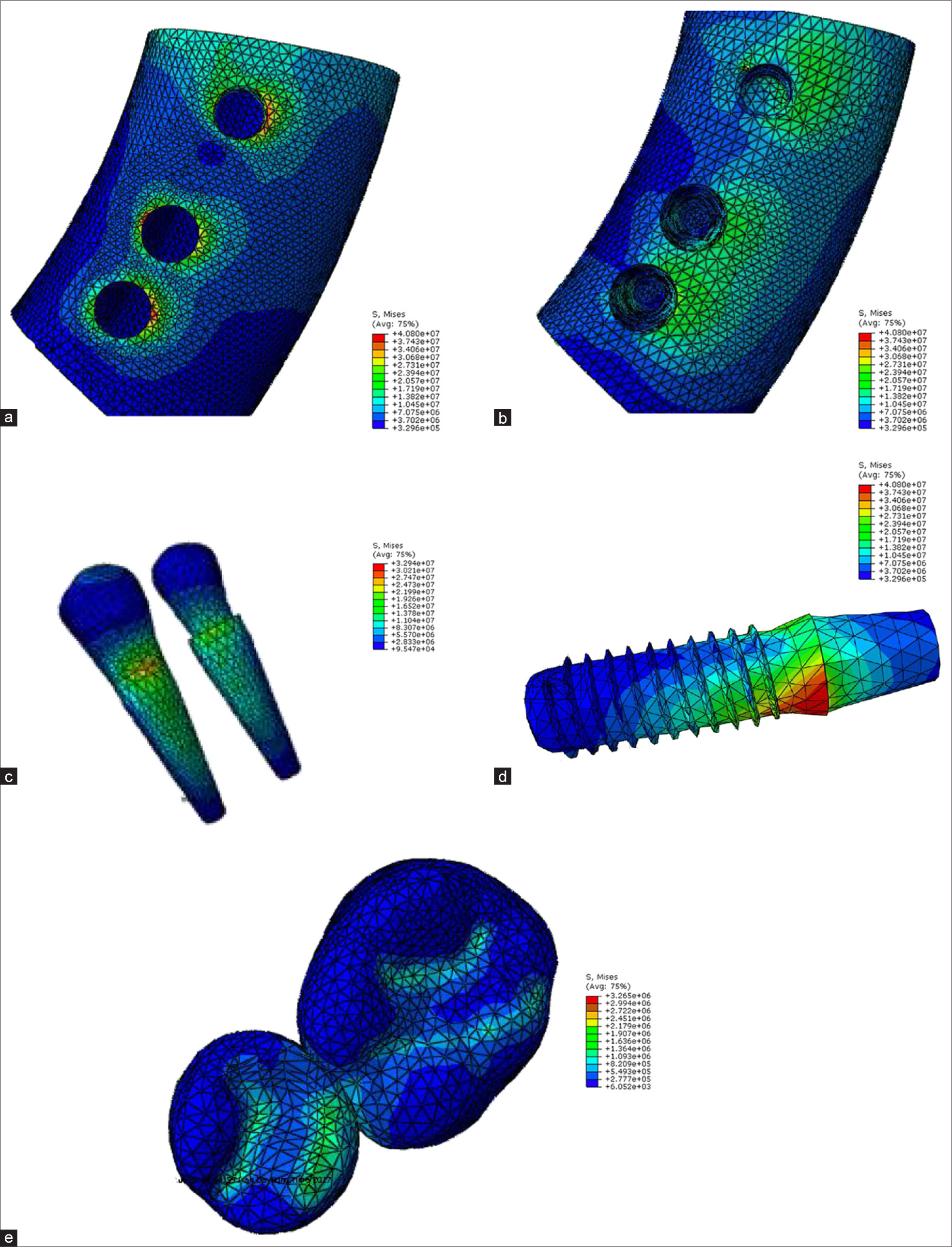
- Model B, force angle 45 (a) Cortical bone, (b) cancellous bone, (c) teeth 4 and 5, (d) implant, (e) crown.
Model A:
At 0 and 15°, the highest stress is related to the implant crown. At 45°, the highest stress is related to the implant, equal to 80.1 megapascal (MPa).
Model B:
At 0°, 15°, and 45°, the highest stress is related to Tooth 5. The stress level in Tooth 5 at 0° is equivalent to 36.6, at 15° is equivalent to 36.9, and at 45°, it is 70 Mega Pascals.
Comparison of force angles shows that in both models, the stress created in the crown, implants, Tooth 4, and Tooth 5 with a force of 100 Newtons increases at angles of 0, 15, and 45° relative to the bone crystal surface, and the least stress is created by the force at 0° on the bone surface.
The stress level in cortical bone with a force of 100 Newtons increases at angles of 0, 15, and 45° relative to the bone surface in Model 1 but initially decreases and then increases with an increase in the angle in Model 2. The stress level in trabecular bone with a force of 100 Newtons increases at angles of 0, 15, and 45° relative to the bone surface in Model 1, with an initial increase and then decrease with an increase in the angle, but in Model 2, it increases with an increase in the angle.
In addition, in the comparison of the two models studied, in Model A, the implant with a cantilevered coating, the stress created in the Crown and implant is greater than the stress created in Model B, and the stress created in Tooth 5 is less in Model A.
DISCUSSION
In this study, a force of 100 Newtons was applied at three different angles (0, 30, and 45°) relative to the crestal surface to reconstruct undesirable forces. The stress distribution was evaluated using FEA, which is a computer-based method in vitro to create fully clinical conditions that are not practical. The study aimed to investigate the consequences of connecting implants with cantilevered crowns to reduce the adverse effects of cantilevers. The results showed that when implants were connected to teeth with cantilever crowns, the stress on the implant and implant crown decreased at all angles, consistent with previous studies.[25,26]
The maximum stress level in cortical and cancellous bone was observed in model A with the angle of 45 and 15°, respectively, while the least stress level was obtained at 15 and 0° for model B. Increasing the angle of force direction from 0 to 15 resulted in a decrease in the amount of stress for model B, while the stress level showed increased levels of stress by changing the angle from 0 to 15. Increasing the angle to 45° resulted in an increase in the stress level for both models. Considering the cancellous bone, increasing the angle of force direction from 0 to 15 and 15 to 45° resulted in an increase in the amount of stress for model B, while the stress level showed increased levels of stress by changing the angle from 0 to 15 and a subsequent decrease by changing the angle to 45° in model A.
The results also indicated that stress concentration was higher in cortical bone compared to the cancellous bone, consistent with Udomsawat et al., findings that assessed the stress distribution patterns around three distinct dental implant models as they are being inserted into the bone, employing dynamic finite element stress analysis and concluded that the stress levels within the cancellous bone were significantly lower than those in the cortical bone, attributable to the distinct material properties of each bone type.[27]
Stress distribution in implant and the implant’s crown: The amount of stress distribution for both the implant and the implant’s crown was highest at 45° and it was higher in model A compared to model B at all force angulations. Similarly, Lemos et al. evaluated stress distribution in the implants/components and bone tissue for splinted and non-splinted prostheses with different lengths of implants using 3-D FEA. They concluded that splinted prostheses contributed to better stress distribution in the implant/abutment and cortical bone tissue; however, the reduction in the implant length did not influence the stress distribution.[28]
Stress distribution in tooth 4 and 5: The amount of stress distribution for both teeth showed a continuous increase from 0 to 15 and to 45° of force direction; however, the amount of increase in model B was more considerable. These results are consistent with that of previous studies, which also reported that splinted crowns improve the sharing of stress with adjacent implants in other implant connections.[29] The advantage of splinted crowns in sharing stress with other implants/teeth could be explained by the rigid union of components, which enables the stress distribution between implants/teeth. In the present study, a rigid connector was also used to connect the tooth and implant.
Hoffmann and Zafiropoulos (2012) investigated the long-term effects of restorations supported by implants and natural teeth, considering the effects of implants, teeth, and their restoration on the connector used. Authors reported that the use of rigid connectors resulted in better clinical outcomes in long-term stability, reduced complications, and dental intrusion. In addition, the study revealed that the combination of teeth and implants for supporting restorations has less long-term success compared to using implants alone.[23] Similarly, Chee and Mordohai (2010) found that among various types of connections, rigid connections showed fewer complications, although not completely eliminating them.[30]
The topic of tooth and implant connection is debatable, with some articles considering such connections detrimental[31] while others, taking specific considerations into account, find them unobstructive.[32]
Based on the results, stress concentration in both models was around the implant neck and decreased apically, aligning with Menicucci’s findings.[25] Menicucci et al. demonstrated that when temporary pressure is applied to a tooth, both the implant and its associated tooth share the pressure, distributing the applied stress in the surrounding bone.[25]
While attempting to simulate clinical specimens using FEA, several limitations emerged. The dimensions of the supra-structures were obtained from real clinical samples, and the implant sizes were sourced from commercial suppliers to ensure realistic model geometries. However, the study assumed that the structures were homogeneous and isotropic and that the bone-implant interface was fully osseo-integrated. These assumptions are recognized as limitations of the study.
CONCLUSION
Within the limitations of this study, we conclude that splinted prostheses contributed to better stress distribution in the implant, cortical, and cancellous bone tissue; however, the tooth will be under more stress when connected to the implant. The claim in the conclusion – that attachment of dental implants to adjacent teeth is a suitable alternative for patients with challenging anatomical considerations – is supported by our FEA results, which demonstrated significant reductions in stress levels when the implant was connected to adjacent teeth. Specifically, Model B, with a pontic connected to both an implant and a tooth abutment, showed lower stress levels (58.26 MPa in the implant and 35.8 MPa in the crown) compared to Model A (80.1 MPa in the implant and 66.5 MPa in the crown) under a 100N force at a 45° angle. This indicates a more favorable distribution of forces and reduced biomechanical complications, aligning with existing literature that highlights the benefits of splinted prostheses in stress distribution and clinical outcomes. However, in this type of connection, the tooth adjacent to the implant experiences more stress because the forces applied to the prosthesis are transferred to the adjacent tooth, resulting in increased pressure and stress concentration in that tooth. These findings validate the clinical relevance and effectiveness of using combined implant-tooth connections, particularly in anatomically constrained scenarios.
Ethical approval
The research/study is approved by the Institutional Ethics Committee at Ahvaz Jundishapur University of Medical Sciences, number IR.AJUMS.REC.1397.200, dated 09th June 2018.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Dual jaw treatment of edentulism using implant-supported monolithic zirconia fixed prostheses. J Esthet Restor Dent. 2015;27:63-70.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term treatment outcomes of implant prostheses in partially and totally edentulous patients. Materials (Basel). 2022;15:4910.
- [CrossRef] [PubMed] [Google Scholar]
- The etiology and management of dental implant failure: A review. Cureus. 2022;14:e30455.
- [CrossRef] [PubMed] [Google Scholar]
- Stress-absorbing elements in dental implants. J Prosthet Dent. 1990;64:198-205.
- [CrossRef] [PubMed] [Google Scholar]
- An investigation of tooth/implant-supported fixed prosthesis designs with two different stress analysis methods: An in vitro study. J Prosthodont. 2007;16:107-16.
- [CrossRef] [PubMed] [Google Scholar]
- Numerical simulation on the biomechanical interactions of tooth/implant-supported system under various occlusal forces with rigid/non-rigid connections. J Biomech. 2006;39:453-63.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional finite element analysis of the stress distribution around the implant and tooth in tooth implant-supported fixed prosthesis designs. J Dent Implants. 2011;1:75-9.
- [CrossRef] [Google Scholar]
- Considerations preliminary to the application of early and immediate loading protocols in dental implantology. Clin Oral Implants Res. 2000;11:12-25.
- [CrossRef] [PubMed] [Google Scholar]
- Complications in implant dentistry. Eur J Dent. 2017;11:135-40.
- [CrossRef] [PubMed] [Google Scholar]
- The biomechanics of implant-supported cantilevered fixed partial dentures: Systematic review of the literature. Oral Health Care. 2020;5:1-5.
- [CrossRef] [Google Scholar]
- Clinical study on screw loosening in dental implant prostheses: A 6-year retrospective study. J Korean Assoc Oral Maxillofac Surg. 2020;46:133-42.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanical stress during implant surgery and its effects on marginal bone: A literature review. Quintessence Int. 2020;51:142-50.
- [Google Scholar]
- Effect of offset implant placement on the stress distribution around a dental implant: A three-dimensional finite element analysis. J Oral Implantol. 2015;41:646-51.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluating parameters of osseointegrated dental implants using finite element analysis--a two-dimensional comparative study examining the effects of implant diameter, implant shape, and load direction. J Oral Implantol. 1998;24:80-8.
- [CrossRef] [PubMed] [Google Scholar]
- Finite element analysis: A boon to dentistry. J Oral Biol Craniofac Res. 2014;4:200-3.
- [CrossRef] [PubMed] [Google Scholar]
- An investigation of three types of tooth implant supported fixed prosthesis designs with 3D finite element analysis. J Dent (Tehran). 2013;10:51-63.
- [Google Scholar]
- Application of finite element analysis in implant dentistry London: IntechOpen; 2012.
- [Google Scholar]
- Tooth-implant connection: A review. J Oral Implantol. 2012;38:194-200.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of prosthesis length and implant diameter on the stress distribution in tooth-implant-supported prostheses: A finite element analysis. Int J Oral Maxillofac Implants. 2012;27:e19-28.
- [Google Scholar]
- Tooth-implant connection: Some biomechanical aspects based on finite element analyses. Clin Oral Implants Res. 2002;13:334-41.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of implant angulation and splinting on stress distribution in implant body and supporting bone: A finite element analysis. Eur J Dent. 2015;9:311-8.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study of stress characteristics in surrounding bone during insertion of dental implants of three different thread designs: A three-dimensional dynamic finite element study. Clin Exp Dent Res. 2018;5:26-37.
- [CrossRef] [PubMed] [Google Scholar]
- Splinted and nonsplinted crowns with different implant lengths in the posterior maxilla by three-dimensional finite element analysis. J Healthc Eng. 2018;2018:3163096.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of the biomechanical behavior of short implants: The photo-elasticity method. Mater Sci Eng C Mater Biol Appl. 2015;55:187-92.
- [CrossRef] [PubMed] [Google Scholar]
- Tooth-to-implant connection: A systematic review of the 62 literature and a case report utilizing a new connection design. Clin Implant Dent Relat Res. 2010;12:122-33.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of different implants on the biomechanical behavior of a tooth-implant fixed partial dentures: A three-dimensional finite element analysis. J Oral Implantol. 2020;46:27-34.
- [CrossRef] [PubMed] [Google Scholar]
- Survival and complication rates of tooth-implant versus freestanding implant supporting fixed partial prosthesis: A systematic review and meta-analysis. J Prosthodont Res. 2021;65:1-10.
- [CrossRef] [PubMed] [Google Scholar]