Translate this page into:
Endodontic and surgical management of traumatic radicular cyst: A case report
*Corresponding author: Prachi Anil Choudhari, Department of Conservative Dentistry and Endodontics, Ranjeet Deshmukh Dental College and Research Center, Nagpur, Maharashtra, India. prachichoudhary26995@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Choudhari PA, Shenoi PR, Gunwal MK, Shahu S. Endodontic and surgical management of traumatic radicular cyst: A case report. J Adv Dental Pract Res. 2024;3:27-31. doi: 10.25259/JADPR_36_2024
Abstract
A radicular cyst is most common among all cystic lesions of the jaw. It is mostly associated with apical and lateral exits of an infected root canal. Radicular cysts are usually asymptomatic and often discovered accidentally on routine radiographic examination. This article presents a case of 18 years old male patient with the chief complaint of palatal swelling for a month and history of trauma. Based on clinical, radiological and cytological examination, a provisional diagnosis of infected radicular cyst was made. The treatment plan included root canal therapy followed by surgical enucleation of cystic lesion and apicectomy of the involved tooth. Patient remained asymptomatic in follow up period and 18 months follow up radiographs showed complete resolution of periapical radiolucency and new bone formation at the site of cystic lesion.
Keywords
Radicular cyst
Non vital tooth
MTA
Cysts
Trauma
INTRODUCTION
A radicular cyst is the most frequently occurring cystic lesion of the jaw. It is a usual but not inevitable sequela of periapical granuloma originating as a result of bacterial infection and necrosis of dental pulp nearly always following carious involvement of the tooth (Shafers, 1993). It is commonly associated with the apical and lateral openings of the infected root canal. Usually asymptomatic, radicular cysts are often discovered only during routine radiographic examinations. Although symptomatic, their acute exacerbation of the long-term lesion can lead to tooth mobility, swelling, and displacement of adjacent teeth. The radiographic appearance of most of them is a round and uniform radiolucent lesion with or without the presence of sclerotic borders. Histological examination is crucial to confirm the diagnosis of radicular cysts. Treatment options for radicular cysts vary, ranging from conventional nonsurgical root canal therapy for smaller cysts to surgical approaches such as enucleation, marsupialization, or decompression for larger cysts.[1]
CASE REPORT
An 18-year-old male patient with the chief complaint of palatal swelling for a month and a history of trauma 8 years ago reported to our department. Intraoral examination revealed a round and well-defined swelling, measuring 2–3 cm in size and extending from the anterior palatine rugae to the junction of the hard and soft palate on the left side without crossing the midline [Figure 1]. The swelling was fluctuant in nature, tender on palpation and associated with purulent discharge. 21, 22, and 23 were slightly tender on vertical percussion and showed no response to vitality testing. Grade I mobility was noted with 21.

- Pre-operative intraoral view.
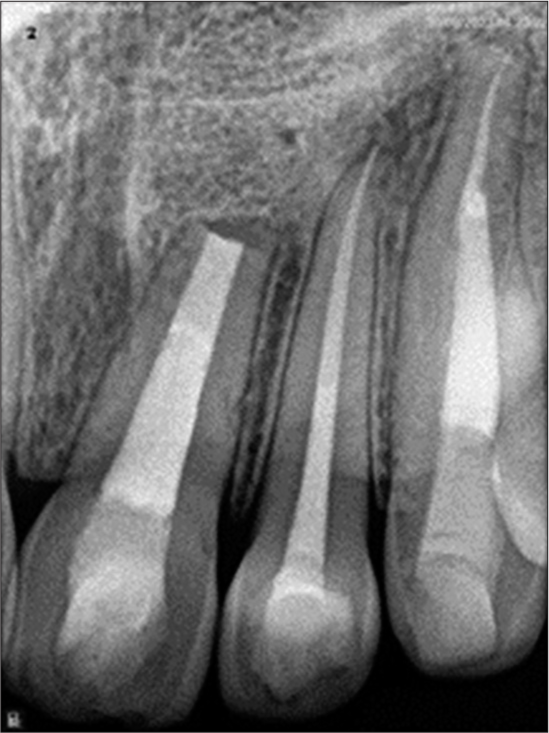
On radiographic investigations, a large, unilocular radiolucent lesion involving the apices of 21, 22, and 23 was noted. Incomplete root formation was seen with 21 [Figure 2]. Cone-beam computed tomography revealed palatal plate perforation and thinning of the nasal floor as additional findings. Fine-needle aspiration cytology showed yellowish-brown colored turbid fluid containing acute inflammatory cells infiltrate, prominently neutrophils indicative of an acute inflammatory lesion. A preliminary diagnosis of an infected radicular cyst was established based on clinical examination, radiological findings, and aspirate analysis.
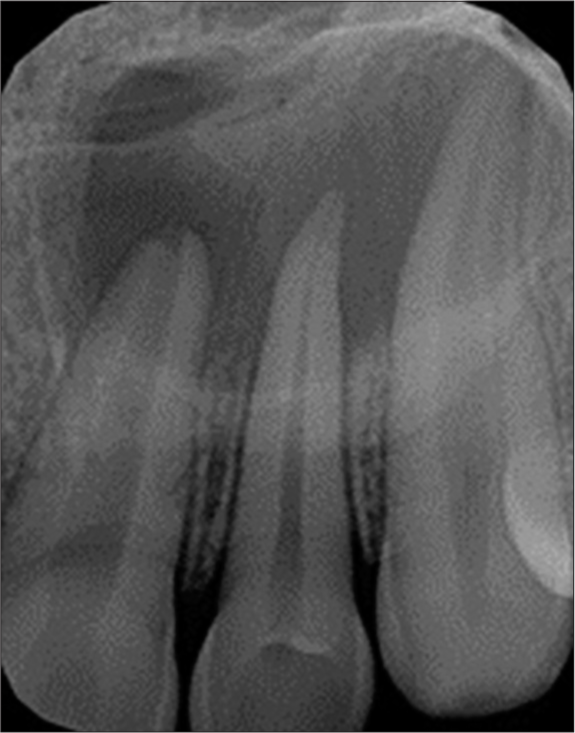
- Pre-operative periapical radiograph.
The treatment plan included root canal therapy for 21, 22, and 23, along with the creation of a root end barrier with 21 using mineral trioxide aggregate (MTA). This was followed by surgical enucleation of the cystic lesion and apicectomy of 21. After the patient’s informed consent, root canal treatment was initiated under local anesthesia using rubber dam isolation. After access cavity preparation and working length determination, biomechanical preparation was carried out with the Azure Endostar E3 file system along with copious irrigation with normal saline, 17% ethylenediaminetetraacetic acid (EDTA) and 2.5% sodium hypochlorite. After proper drying of the canals, an intracanal non-setting calcium hydroxide dressing was placed and access cavities were sealed for 10 days. In the second visit, 22 and 23 were obturated. As 21 presented with wide open apex, MTA (PROROOT MTA, Dentsply Sirona) was used to create an artificial apical barrier of 8 mm [Figure 3].
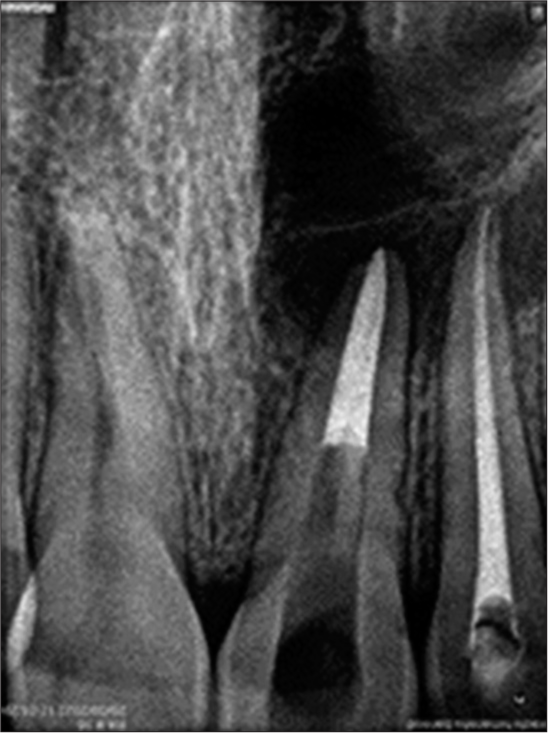
- Root end barrier with mineral trioxide aggregate (MTA).
On the following day, periapical surgery was carried out under magnification. The operating site was anesthetized with 2% lignocaine with epinephrine (1:100,000). A sulcular incision was made followed by raising a full-thickness mucoperiosteal flap with two vertical releasing incisions on either side. The cystic lesion was enucleated and curetted. Apicectomy was performed with 21 [Figure 4]. Flap repositioning and closure were carried out with 3–0 silk sutures (Ethicon Mersilk). The obtained periapical specimen was sent for histological analysis. The histopathological features were consistent with the preliminary diagnosis of an infected radicular cyst. The lining of the cystic cavity consisted of non-keratinized stratified squamous epithelium. Adjacent to the cystic cavity, the connective tissue wall was fibro-cellular, consisting of fibroblasts and fibrocytes with severe chronic inflammatory infiltrates [Figure 5].

- Apicectomy.
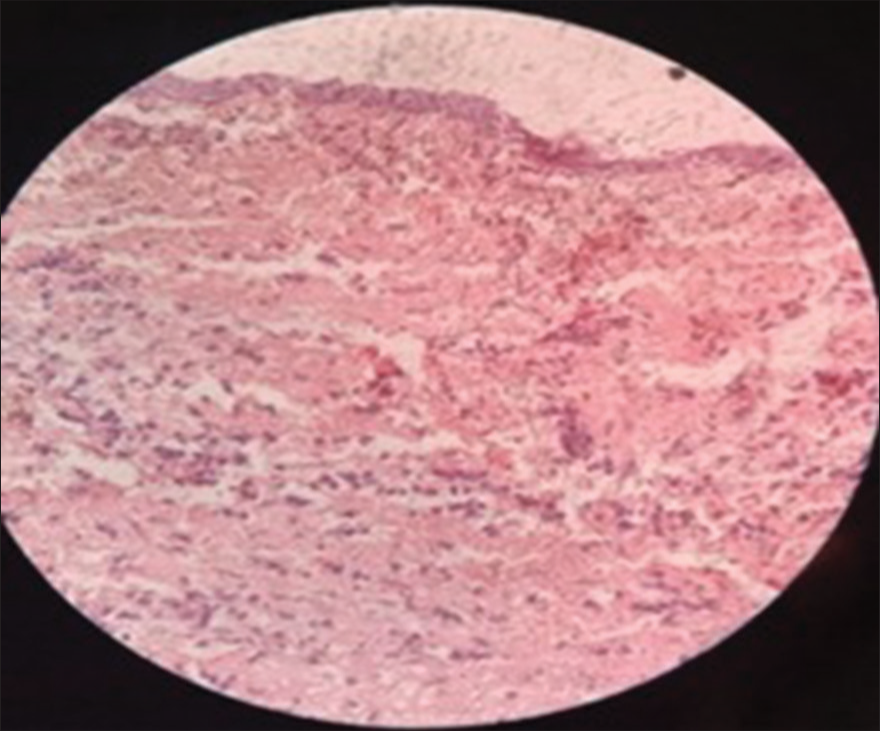
- Histopathological analysis.
The patient was given post-operative instructions and prescribed antibiotics and analgesics. The patient was recalled after 7 days for follow-up. After initial soft-tissue healing, 21 was obturated with thermoplasticized guttapercha. Post-endodontic restoration was completed with 21, 22, and 23 using a nanohybrid composite (Kulzer Charisma smart hybrid).
The patient remained asymptomatic in the follow up period and showed a complete resolution of swelling. At 6-month follow-up, periapical radiographs showed resolution of periapical radiolucency, and 24-month follow-up radiographs revealed complete healing with bone formation at the location of the cystic lesion [Figure 6].
- Follow-up periapical radiograph.
DISCUSSION
A cyst is characterized as a pathological cavity that may or may not be lined with epithelium and typically grows centrifugally in an expansive manner. Among all odontogenic cysts of the jaws, the radicular cyst is the most common type, with 9% being true cysts and 6% being pocket cysts. Its prevalence peaks during the third decade of life and males are more commonly affected than females. The most common site of occurrence is the maxillary anterior region.[2] The current report presents a case of an 18-18-year-old male with a lesion in the maxillary anterior region.
Trauma is one of the etiological factors for radicular cysts. Trauma leads to necrosis of the pulp and renders teeth non-vital. Long-standing untreated pulpal infections result in the development of a periapical cyst. The patient had a history of trauma in the anterior region and 21, 22, and 23 were non-vital. It has been observed that continued cyst expansion can lead to the non-vitality of adjacent teeth.[3] These findings suggest that trauma could be the possible etiology for the non-vitality of teeth and the development of a radicular cyst in the present case.
The pathophysiology of radicular cysts involves three distinct phases: Initiation, cyst formation, and growth. Being usually asymptomatic, they are often discovered incidentally on radiographs. However, in long-standing cases, these cysts may exhibit characteristic features, with acute exacerbations causing symptoms such as swelling, displacement of adjacent teeth, root resorption, and mobility of the affected teeth. In late stages, cortical enlargement along with bone resorption may lead to a phenomenon known as eggshell crackling.[4] In the current case, the patient was asymptomatic except for mild sensitivity with 21. However, the patient developed palatal swelling and pain following an acute exacerbation of the lesion.
Radiographically, radicular cysts appear as osteolytic lesions with well-corticated borders. However, in cases of infection or rapid enlargement, the radiopaque margin may be absent or not clearly visible. This could potentially explain the radiological appearance of the present case, as the lesion showed no corticated borders, and the swelling rapidly developed following an acute exacerbation without any subperiosteal bone formation. In addition, the presence of palatal plate perforation and thinning of the nasal floor, which are the common manifestations of cyst expansion were also observed.
The treatment approach often depends on several factors, including the cyst’s location, the integrity of its wall, its size, and its proximity to vital structures. In the current case, root canal treatment was initiated with 21, 22, and 23 as they were non-vital. Thorough chemical-mechanical debridement was done to eliminate the necrotic pulp and bacterial products. The irrigation protocol for non-vital teeth, that is, 2.5% sodium hypochlorite along with saline and 17% EDTA was followed.[5] Intracanal calcium hydroxide dressing was placed as an intracanal medicament for 10 days as it maintains a high pH in periapical tissues and promotes and accelerates the healing process.
As an open apex was seen with 21, MTA was used to create an artificial apical barrier. Panda et al., in their systematic review and meta-analysis, have shown that MTA stands as a promising biomaterial to be used as a root end barrier due to its excellent biocompatibility, better sealing ability, less microleakage, bactericidal effects, and good radiopacity.[6]
The conservative approach entails removing infected tissues, whereas procedures such as en bloc resection involve removing both diseased and normal structures. Surgical management options for jaw cysts typically include marsupialization or enucleation. The type of cyst also significantly influences treatment planning: true cysts are self-sustaining and may persist despite treatment of infected tooth. In contrast, pocket cysts have a lumen connected to the root canal and rely on pulpal and periapical infection for their growth and persistence. Therefore, pocket cysts typically regress after root canal treatment, whereas true cysts necessitate surgical removal. In the current case, surgical enucleation and curettage were considered. Root end resection with 21 was also carried out as it was noted as the focus of infection. A 3 mm root end was resected as suggested by Kim and Kratchman because 93% of lateral canals and 99% of ramifications are believed to be present in the apical 3 mm of root.[7]
To accelerate the healing process, guided bone regeneration methods are employed following surgical enucleation. However, there is debate surrounding their use in periapical defects. Some studies suggest that regenerative techniques do not necessarily offer superior speed or quality of healing.[8] Conversely, other research indicates that cases treated with regeneration methods show more predictable outcomes compared to conventional treatments.[9,10] In our specific case, we observed complete bone regeneration without utilizing any guided tissue regenerative techniques.
The histopathological analysis of the obtained specimen during enucleation was in accordance with the clinical diagnosis of an infected radicular cyst. The cystic lesion consisted of a non-keratinized, stratified squamous epithelium lining. Histopathological analysis in a study indicated that 98.3% of radicular cysts featured a non-keratinized stratified squamous epithelial lining. Mucoepidermoid and respiratory epithelia were present in 0.9% of cases and 0.4% of cases showed epithelial dysplastic features. At present, no strong evidence suggests that cystic epithelium is prone to carcinomatous transformation, nor is there justification for categorizing cysts in the category of precancerous lesions. Some cases have reported hyaline bodies. Cholesterol crystal deposits form due to the degradation of red blood cells (RBCs), macrophages, white blood cells, and plasma cells. In the present case specimen, histopathological analysis showed acute and chronic inflammatory infiltrates without the presence of Rushton bodies. Mild-to-moderate vascularity with extravasated RBCs was observed. Toward the periphery, the connective tissue wall exhibited a parallel arrangement of collagen fiber bundles alongside osseous trabeculae.
In the present case, the patient remained asymptomatic during the follow-up period and 24 months of follow-up radiographs revealed complete resolution of periapical radiolucency and bone formation at the location of the cystic lesion.
CONCLUSION
The radicular cyst is the predominant inflammatory odontogenic cyst that usually develops following trauma or dental caries. Accurate diagnosis of radicular cysts necessitates comprehensive evaluation through histopathological, clinical, and radiological assessments. Therefore, this case report on the radicular cyst provides an overview of its clinical, histological, and radiological characteristics, as well as its treatment approach.
Acknowledgement
The authors would like to thank the Department of Conservative Dentistry and Endodontics, Ranjeet Deshmukh Dental College and Research Center, Nagpur.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Pratima R. Shenoi and Dr. Mohit K. Gunwal are on the Editorial Board of the Journal
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Management of large radicular cyst by conservative surgical approach: A case report. J Clin Diagn Res. 2014;8:239-41.
- [CrossRef] [PubMed] [Google Scholar]
- Conservative non-surgical management of an infected radicular cyst. Contemp Clin Dent. 2011;2:368-71.
- [CrossRef] [PubMed] [Google Scholar]
- Preserving the vitality of teeth adjacent to a large radicular cyst in periapical microsurgery: A case report with 4-year follow-up. BMC Oral Health. 2021;21:382.
- [CrossRef] [PubMed] [Google Scholar]
- Radicular cyst: A cystic lesion involving the hard palate. Cureus. 2023;15:e47030.
- [CrossRef] [Google Scholar]
- Effectiveness of intracanal calcium hydroxide medicament in treating periapical lesions: A systematic review. J Stomatol. 2022;75:44-54.
- [CrossRef] [Google Scholar]
- Clinical outcome and comparison of regenerative and apexification intervention in young immature necrotic teeth-a systematic review and meta-analysis. J Clin Med. 2022;11:3909.
- [CrossRef] [PubMed] [Google Scholar]
- Modern endodontic surgery concepts and practice: A review. J Endod. 2006;32:601-23.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of xenogeneic bone grafting with guided tissue regeneration in the management of bone defects after surgical endodontics. J Oral Maxillofac Surg. 2007;65:1121-7.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of healing process of bone defects after apicectomy: Results after 6 and 12 months. J Physiol Pharmacol. 2009;60(Suppl 8):51-5.
- [Google Scholar]
- Guided bone regeneration (GBR) using membranes and calcium sulphate after apicectomy: A comparative histomorphometrical study. Int Endod J. 2002;35:255-63.
- [CrossRef] [PubMed] [Google Scholar]