Translate this page into:
Evaluation of awareness and knowledge about medication-related osteonecrosis of jaws among interns and postgraduates: A cross-sectional study
*Corresponding author: Nidhi Jayant Khangar, Department of Oral and Maxillofacial Surgery, VSPM’s Dental College and Research Center, Nagpur, Maharashtra, India. nidhikhangar30@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Khangar NJ, khandaitkar S, Shenoi R. Evaluation of awareness and knowledge about medication-related osteonecrosis of jaws among interns and postgraduates: A cross-sectional study. J Adv Dental Pract Res 2022;1:57-63.
Abstract
Objectives:
Osteonecrosis is a common terminology used nowadays associated with severe trauma. Osteonecrosis also known as avascular necrosis occurs due to diminished blood supply, depriving bone tissue of essential nutrients, and oxygen leading to death of bone cells in a circumscribed region. Medication-related osteonecrosis of jaws (MRONJs) are a recent concept and correspond to necrosis of bones particularly jaw bones due to use of certain medications without any prior exposure to radiation. Several medications tend to alter the bone remodeling process, affecting the diseased bone resorption, and leading to poor oral health maintenance. Adequate documentation and awareness about this condition can help to prevent the condition. This study aims to evaluate the existing knowledge that prevails about pathogenesis, staging, and treatment modalities currently available about the condition among interns and postgraduates.
Materials and Methods:
An online questionnaire-based cross-sectional survey was carried out among interns and postgraduates of VSPM’s Dental College and Research Center. General characteristics, knowledge about medications responsible, pathogenesis, risk factors, staging, treatment protocols, and drug holiday were recorded that the responses were compiled and statistically analyzed.
Results:
A total of 125 participants participated in the survey. About 72.8% of participants had heard about this condition earlier, whereas 8.8% were unaware of this terminology. About 27.2% people had no idea about the drug holiday concept. Furthermore, significant difference existed between designation and responses.
Conclusion:
The results suggest that a significant difference exists between awareness about MRONJ among interns and postgraduates. Postgraduate students currently pursuing their degree were more aware and had significant knowledge about the clinical entity and more inclined toward further upgrading their knowledge about the same rather than interns.
Keywords
Medication-related osteonecrosis of jaws
Drug holiday
Anti-osteoporotic
Interns
Postgraduates
Bisphosphonates
INTRODUCTION
Medication-related osteonecrosis of jaws (MRONJs) are debilitating clinical entity characterized by non-healing exposed bone associated with the use of anti-osteoporotic drugs primarily bisphosphonates without any prior exposure to radiation in the head and neck region. It refers to progressive bone death. It is an uncommon side effect seen in some individuals.
Marx, in 2003, reported the first instance of the condition as a side effect in a patient receiving bisphosphonate treatment.[1,2] Therefore, earlier this entity was known as BRONJ, bisphosphonate-related osteonecrosis of jaws. An update was made in 2014 by AAOMS to change the tem from BRONJ to MRONJ following many case reports of progressive bone death associated with anti-angiogenic and anti-resorptive drugs usage.[1] The prevalence of disease is very low, but its likelihood in cancer patients is 0–12%.
Several drugs have an impact on the bone loss process. These bone modifying drugs can lead to MRONJ. MRONJ is seen to be associated with anti-osteoporotic, anti-angiogenic drugs, and anti-resorptive drugs such as bisphosphonates and denosumab, selective estrogen receptors, and RANKL but more commonly is seen to be associated with bisphosphonates and denosumab which are also the two most frequently prescribed drugs for osteoporosis.[1]
Pathogenesis of the condition is not entirely understood till now but also it is hypothesized that the drugs interferes with osteoclast activity, altering the bone healing and remodeling process. Furthermore, they also inhibit angiogenesis. Tooth extraction and dentoalveolar surgeries are considered to be significant risk factors for MRONJ to develop.[1] The clinical evidence of necrotic bone for more than 8 weeks without healing is an indicator for the disease.
The side effects of bisphosphonate on bones even after discontinuation of the drug are an important reason to consider “DRUG HOLIDAY” for 3–5 years in patients on long-term bisphosphonates therapy. Drug holiday is not necessary for patients on denosumab as their effects do not persist after discontinuation.[1]
Since the necrotic effects of bone have not been observed outside bones of craniofacial region, dentists are essential in diagnosis and prevention of this entity this emphasizes the need to spread awareness among dental professionals. Treatment modalities are continuously being upgraded and newer research is being done on the topic. Therefore, it is essential that the future dental surgeons are aware and prepared to handle the condition and provide a better treatment protocol to their patients. The overarching aim of this study is to enhance knowledge of the dental professionals and draw their attention for further research about treatment protocols and newer advancements in this field.
Aims and objectives
This study aims to evaluate the existing knowledge that prevails about pathogenesis, staging, and treatment modalities currently available about the condition among interns and postgraduates and whether they are aware of the serious complications of the condition.
MATERIALS AND METHODS
A cross-sectional study was conducted in VSPM’s Dental College and Research Center among interns and postgraduates. Ethical clearance was obtained from the Institutional Ethics Committee of VSPM’s Dental College and Research Center; approved no IEC/VSPMDCRC/76/2022. A total of 125 participants participated in the study among which 96 were interns and 29 participants were postgraduate students studying in the VSPM educational academy campus. An online self-administered questionnaire was circulated from the month of June to August, and after recording 125 responses, the link was closed. Data collection was done from all the willing participants. The questionnaire recorded the demographic data, medications responsible, frequency of involvement, pathogenesis, staging, drug holiday administered, and treatment modalities available about the clinical entity. Data were collected using Google forms and were compiled in Excel Sheet and statistically analyzed using IBM SPSS 2020 Software. Test of significance used was Chi-square test to compare the values between the two groups.
RESULTS
A total of 125 responses were collected. Range of age of the participants was between 22 and 28 years. Mean age was 23 years [Figure 1]. Among these 71.2% were female and the rest 28.8% were male [Figure 2]. About 76.8% of responses were recorded from interns and 23.2% of responses were from postgraduate group [Figure 3].

- Age of participants.
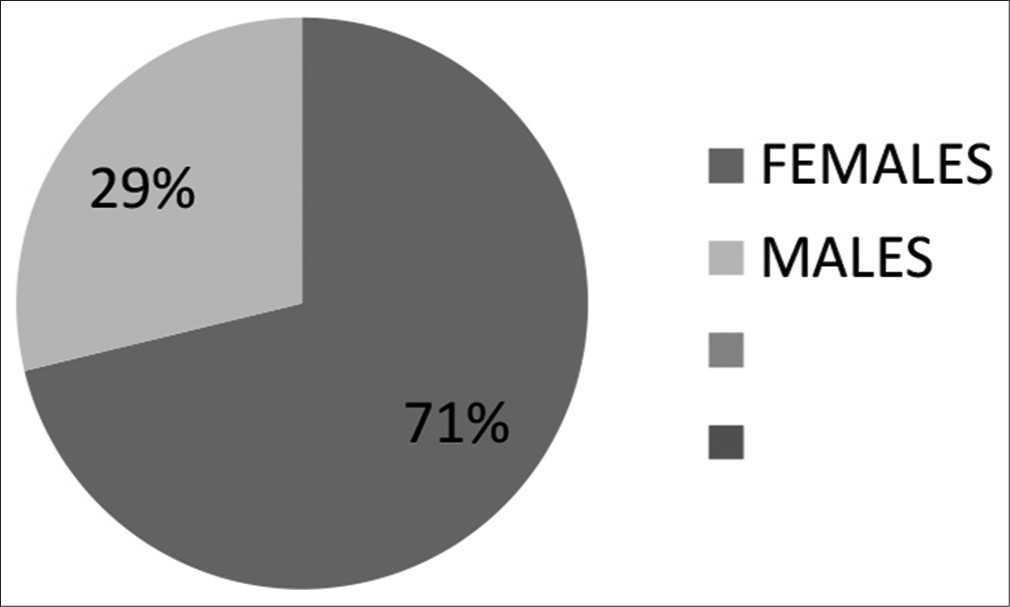
- Gender of participants.

- Designation of participants.
A descriptive analysis is depicted in [Table 1] below:
About 62.4% of students were aware about all the drugs causing osteonecrosis, whereas 20.8% of participants were only aware of bisphosphonates drug causing osteonecrosis. About 8.8% responders voted for denosumab and 8% of them thought that it is a side effect of anti angiogenic drugs. About 56% of students were in favor of mandibular involvement, whereas 16% favored maxillary involvement. About 13.6% of students were however not aware about which jaw bone was more affected and 14.4% of responders took a toll with equal in both the jaws.
| Descriptive statistics: Demographics | ||
|---|---|---|
| Frequency | Percent | |
| Gender | ||
| Female | 89 | 71.2 |
| Male | 36 | 28.8 |
| Total | 125 | 100.0 |
| Designation | ||
| Intern | 96 | 76.8 |
| Postgraduate | 29 | 23.2 |
| Age | ||
Mean±SD: 23.96±1.24
About 36.8% of participants responded inhibition of osteoclast differentiation as a pathogenesis, 32% of participants favored inhibition of osteoblast differentiation as pathogenesis involved, 22.4% of participants responded with interference in bone remodeling, and 8.8% of individuals favored angiogenesis.
About 37.6% of participants were aware of the staging criteria used that are four stages existed for the condition, while 31.2% of participants responded that clinical entity consist of three staging system. A large population of 24.8% of participants, however, were not aware of the staging criteria, and 6.4% of participants responded to two stages.
Only 38.4% of students knew the drug holiday concept and the recommended drug holiday prescribed, while 10.4% people, 27.2% of participants had no idea about the concept of drug holiday. About 24% of population thought that drug holiday referred to non-availability of drug.
About 35.2% of students responded to >8 weeks duration for MRONJ to occur, 24.8% of students were not aware about the duration of MRONJ to occur, and 18.5% of responders responded with 5 weeks of duration, while the rest 21.6% responded 3 weeks.
About 69.9% of responders took a toll with all of the given options, while 13.6% of participants responded cancer or osteoporosis treatment as a risk factor. About 9.6% of participants answered dental implants to be a risk factor and rest 7.2% of participants favored tooth extractions.
About 55.2% of participants responded that the healing of extraction wound is affected in MRONJ cases, while 35.2% of participants were not sure about the affect and 9.6% of participants responded that it does not affect the wound healing process.
About 36% of student responses recorded clinical evidence of necrotic bone as a mainstay of diagnosis, 25.6% of individuals responses recorded non-healing extraction wound for >8 weeks, and 20.8% of individuals responded to radiography, while the rest 17.6% responded to biopsy.
About 65.6% of participants were in favor of surgical as well as conservative treatment modality, 20.8% of participants were not aware of the treatment modalities available, 8.8% of participants favored surgical intervention only, and 4.8% of participants responded with conservative management.
About 38.8% of students responded that surgical intervention is necessary in stages 2 and 3, 26.8% of students responded that surgical intervention is needed in all the stages, and 22.4% of students responded to surgical intervention in stage 3, while the rest 12.8% responded to intervention in stage 2.
Highest response for drug of choice for entity was recorded for metronidazole 40%. About 38.4% of participants responded with penicillin as drug of choice, 12.8% of students responded with clindamycin, and the rest 8.8% of students responded macrolides.
DISCUSSION
This study focuses on the awareness and difference in levels of knowledge between interns and postgraduates. Medication-related osteonecrosis is sequelae which may occur after tooth extraction a most commonly carried out procedure in dentistry, leading to non-healing of extractions wounds. Bisphosphonates and non-bisphosphonates like medications are widely used in management of bone cancer and diseases,[2] and patients on these drugs are at high risk to develop osteonecrosis. Osteonecrosis or avascular necrosis is nor a specific disease entity, bur rather a condition leading to death of bone tissue in circumscribed region.[3] Therefore, it is necessary to evaluate whether or not awareness and proper treatment protocols are known to future clinicians and bring about their attention toward this clinical entity so that they can promptly identify the patients at risk and efficiently manage the condition. Although, the prevalence is lower than 12% with increasing rise in the administration of these drugs, the prevalence can be suspected to be increased.
A significant difference existed between the knowledge and perceptions of this clinical entity among interns and postgraduates. The response rate of our study was 100% as compared to 46.8% as recorded by Patil et al.[2] About 72.8% of participants had heard about the term MRONJ and aware about the clinical entity. No difference in the awareness about term was observed between intern and postgraduate group. However, the past studies observed that specialized dentists had better understanding.
In the study, awareness of MRONJ among dental professionals: A multicenter study, author recorded that only 31.6% of the participants were aware about the drug holiday concept.[2] However, 38.4% of participants were aware about the concept in our study which signifies the increase in awareness of the dental professionals. Furthermore, among interns and postgraduates, 62% of participants of the postgraduate were aware and only 31.2% were aware among the interns group (P = 0.010) [Table 2]. Similarly, 69.9% of participants of our study were well acquainted with the risk factors, while only 38.5% of the participants were aware in the previous study.[2] Difference between the knowledge among interns and postgraduates was also noted (P = 0.004), [Table 3].
| Descriptive Statistics: Responses | ||
|---|---|---|
| Questionnaire | Frequency | Percent |
| Are you aware of medication-related osteonecrosis of jaws? | ||
| Never heard | 11 | 8.8 |
| No | 23 | 18.4 |
| Yes | 91 | 72.8 |
| Which drugs can cause medication-related osteonecrosis? | ||
| Antiangiogenic drugs | 10 | 8.0 |
| Bisphosphonates | 26 | 20.8 |
| Denosumb | 11 | 8.8 |
| All of the above | 78 | 62.4 |
| Which jaw it affects more? | ||
| Equal frequency in both | 18 | 14.4 |
| Mandible | 70 | 56.0 |
| Maxilla | 20 | 16.0 |
| Not aware | 17 | 13.6 |
| Pathogenesis is related to | ||
| Angiogenesis | 11 | 8.8 |
| Inhibition of osteoblast differentiation | 40 | 32.0 |
| Inhibition of osteoclast differentiation | 46 | 36.8 |
| Interference with bone modeling | 28 | 22.4 |
| Staging includes | ||
| 2 stages | 8 | 6.4 |
| 3 stages | 39 | 31.2 |
| 4 stages | 47 | 37.6 |
| Not aware | 31 | 24.8 |
| Drug holiday concepts is and recommended drug holiday for is | ||
| Drug is no longer available for consumption, 2 months | 30 | 24.0 |
| No idea | 34 | 27.2 |
| When patient stops taking a medication for a period of time, 10 years | 13 | 10.4 |
| When patient stops taking a medication for a period of time, 3–5 years | 48 | 38.4 |
| Duration of MRONJ to occur {minimum} | ||
| 3 weeks | 27 | 21.6 |
| 5 weeks | 23 | 18.4 |
| More than 8 weeks | 44 | 35.2 |
| Not aware | 31 | 24.8 |
| Risk factors for MRONJ include | ||
| All of the above | 87 | 69.6 |
| Dental implants | 12 | 9.6 |
| Patients with ongoing treatment for cancer or osteoporosis | 17 | 13.6 |
| Tooth extraction | 9 | 7.2 |
| Does MRONJ affect healing of extraction wound | ||
| May be | 44 | 35.2 |
| No | 12 | 9.6 |
| Yes | 69 | 55.2 |
| Diagnosis by | ||
| Biopsy | 22 | 17.6 |
| Clinical evidence of necrotic bone | 45 | 36.0 |
| Non-healing extraction wound for >8 weeks | 32 | 25.6 |
| Radiographically | 26 | 20.8 |
| Treatment modalities are | ||
| Can be managed surgically as well as conservatively | 82 | 65.6 |
| Conservative | 6 | 4.8 |
| Not aware | 26 | 20.8 |
| Surgical only | 11 | 8.8 |
| Surgical intervention is required in | ||
| All the stages | 33 | 26.4 |
| Stage 2 | 16 | 12.8 |
| Stage 2 and 3 | 48 | 38.4 |
| Stage3 | 28 | 22.4 |
| First line of choice of antibiotics include | ||
| Clindamycin | 16 | 12.8 |
| Macrolides | 11 | 8.8 |
| Metronidazole | 50 | 40.0 |
| Penicillins | 48 | 38.4 |
MRONJ: Medication-related osteonecrosis of jaws
| Association between designation and responses | |||
|---|---|---|---|
| Questionnaire | Designation | P-value | |
| Intern | Postgraduate | ||
| Are you aware of medication-related osteonecrosis of jaws? | |||
| Never heard | 11.458333 | 0 | 0.004* |
| No | 22.916667 | 3.4482759 | |
| Yes | 65.625 | 96.551724 | |
| Which drugs can cause medication-related osteonecrosis? | |||
| Anti angiogenic drugs | 7.2916667 | 10.344828 | 0.279 |
| Bisphosphonates | 19.791667 | 24.137931 | |
| Denosumab | 11.458333 | 0 | |
| All of the above | 61.458333 | 65.517241 | |
| Which jaw it affects more? | |||
| Equal frequency in both | 16.666667 | 6.8965517 | 0.000** |
| Mandible | 57.291667 | 51.724138 | |
| Maxilla | 8.3333333 | 41.37931 | |
| Not aware | 17.708333 | 0 | |
| Pathogenesis is related to | |||
| Angiogenesis | 10.416667 | 3.4482759 | 0.142 |
| Inhibition of osteoblast differentiation | 30.208333 | 37.931034 | |
| Inhibition of osteoclast differentiation | 33.333333 | 48.275862 | |
| Interference with bone modeling | 26.041667 | 10.344828 | |
| Staging includes | |||
| 2 stages | 7.2916667 | 3.4482759 | 0.000** |
| 3 stages | 31.25 | 31.034483 | |
| 4 stages | 29.166667 | 65.517241 | |
| Not aware | 32.291667 | 0 | |
| Drug holiday concepts is and recommended drug holiday for is | |||
| Drug is no longer available for consumption, 2 months | 25 | 20.689655 | 0.010* |
| No idea | 33.333333 | 6.8965517 | |
| When patient stops taking a medication for a period of time, 10 years | 10.416667 | 10.344828 | |
| When patient stops taking a medication for a period of time, 3–5 years | 31.25 | 62.068966 | |
| Duration of MRONJ to occur {minimum} | |||
| 3 weeks | 26.041667 | 6.8965517 | 0.000** |
| 5 weeks | 20.833333 | 10.344828 | |
| More than 8 weeks | 20.833333 | 82.758621 | |
| Not aware | 32.291667 | 0 | |
| Risk factors for MRONJ include | |||
| All of the above | 61.458333 | 96.551724 | 0.004* |
| Dental implants | 12.5 | 0 | |
| Patients with ongoing treatment for cancer or osteoporosis | 16.666667 | 3.4482759 | |
| Tooth extraction | 9.375 | 0 | |
| Does MRONJ affect healing of extraction wound | |||
| May be | 45.833333 | 0 | 0.000** |
| No | 11.458333 | 3.4482759 | |
| Yes | 42.708333 | 96.551724 | |
| Diagnosis by | |||
| Biopsy | 20.833333 | 6.8965517 | 0.039* |
| Clinical evidence of necrotic bone | 30.208333 | 55.172414 | |
| Non-healing extraction wound for >8 weeks | 25 | 27.586207 | |
| Radiographically | 23.958333 | 10.344828 | |
| Treatment modalities are | |||
| Can be managed surgically as well as conservatively | 56.25 | 96.551724 | 0.002* |
| Conservative | 6.25 | 0 | |
| Not aware | 27.083333 | 0 | |
| Surgical only | 10.416667 | 3.4482759 | |
| Surgical intervention is required in | |||
| All the stages | 33.333333 | 3.4482759 | 0.000** |
| Stage 2 | 15.625 | 3.4482759 | |
| Stage 2 and 3 | 27.083333 | 75.862069 | |
| Stage3 | 23.958333 | 17.241379 | |
| First line of choice of antibiotics include | |||
| Clindamycin | 16.666667 | 0 | 0.013* |
| Macrolides | 11.458333 | 0 | |
| Metronidazole | 35.416667 | 55.172414 | |
| Penicillins | 36.458333 | 44.827586 | |
MRONJ: Medication-related osteonecrosis of jaws, *indicates P value is statistically significant
Similarly, difference in the knowledge and awareness was noted while recording staging (P = 0.000), duration of MRONJ, diagnosis criteria, treatment modalities surgical intervention, and drug choice [Table 3].
It is important that along with dentist, medical professionals should also consider the risk factors while prescribing these medications.[2] Patients are mostly unaware of the drugs that they are prescribed and, hence, may fail to report them during dental examination. Therefore, it is mandatory for the clinician to take a thorough case history and do proper clinical examination for any procedure. This might help to prevent the condition.
The limitations of the study were that only small sample size was included and was conducted in a single institution. Much variation in the responses may not be recorded due to informal discussions among the respondents. The sample size was unequal in both the groups, and hence, the results cannot be extrapolated to all dental professionals.
CONCLUSION
The results imply that postgraduates were more aware about MRONJ as compared to interns. Although a higher level of awareness and knowledge was found in postgraduate group, not all of them were aware about the concept. Furthermore, in depth, understanding about the condition is very important for prevention and treatment of the clinical condition as no effective treatment has been developed till date.[4] Thus, there is need for development of educational interventions and further research to reduce the risk of medication-related osteonecrosis for enhancement of patients health by dental professionals.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- The awareness and practice of dentists regarding medication-related osteonecrosis of the jaw and its prevention: A cross-sectional survey. BMC Oral Health. 2021;21:155.
- [CrossRef] [PubMed] [Google Scholar]
- Awareness about medication-related osteonecrosis of the jaw among dental professionals: A multicentre study. Oral Health Prev Dent. 2020;18:505-9.
- [Google Scholar]
- Osteonecrosis In: Cite as Osteonecrosis: Historical Perspective. Heidelberg: Springer; 2014. p. :3-15.
- [CrossRef] [Google Scholar]
- Awareness of medication-related osteonecrosis of the jaws amongst dental professionals in Poland. Appl Sci. 2021;11:4821.
- [CrossRef] [Google Scholar]