Translate this page into:
Removable overlay dentures: A possible esthetic alternative for the prosthodontic management of partially edentulous skeletal class-3 malocclusions
*Corresponding author: Abeer Babiker Hamad El-Nil, Department of Restorative Dentistry, Thumbay Dental Hospital, Ajman United Arab Emirates. abeer.babiker@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Hamad El-Nil AB. Removable overlay dentures: A possible esthetic alternative for the prosthodontic management of partially edentulous skeletal class-3 malocclusions. J Adv Dental Pract Res. 2024;3:65-9. doi: 10.25259/JADPR_55_2024
Abstract
Skeletal class-3 malocclusions present considerable challenges during dental treatment. Challenges arise from several factors, such as the presence of reverse overjet, anterior or posterior crossbites, open bites teeth relationships, maxillary jaw retrusion, or mandibular jaw protrusion, resulting in functional and esthetic problems. Orthodontic treatment with or without orthognathic surgery is the first recommended treatment of choice. However, the presence of limiting factors, for example, multiple missing teeth, deficient bone, high treatment cost, surgical complications, etc., may not make it a feasible option for all cases. Alternatively, such cases may be managed by a combination of restorative and prosthodontic treatment. This case report presents a skeletal class-3 malocclusion case that was managed by a combination of minimally invasive prosthodontic and restorative treatment approaches that resulted in excellent overall functional and esthetic outcomes.
Keywords
Class-3 malocclusions
Removable partial dentures
Overlay dentures
Overdentures
Increase in vertical dimension
INTRODUCTION
Skeletal class-3 malocclusions are generally one of the most difficult malocclusions to treat in orthodontics.[1] They are usually divided into two categories: dental and skeletal.[2] Features of dental class-3 include lower canines and molars present mesial to their upper counterparts, anterior crossbites, and reverse overjet, generally treated with orthodontics.[3] The chewing ability and bite force of these patients is reduced compared to patients with class-1 malocclusions.[2] They are vertical chewers with vertical envelope of function because the malocclusion does not allow forward mandibular movement.[3] As a result, they do not have anterior or canine guidance.[3] Dental or pseudo-class-3 malocclusions may be treated with only orthodontic treatment or prosthodontic treatment. This is through fixed prosthesis, for example, veneers, crowns, or bridges when the patient refuses long orthodontic treatment or combined for best functional and esthetic results.[4]
Skeletal class-3 is caused by maxillary retrognathia and or mandibular prognathia.[1] In 40% of class-3 patients, maxillary retrognathism is the main cause of the problem.[1] They present with poor facial esthetics due to a concave facial profile, enlarged lower facial third, and protruded lower lip compared to the upper lip.[2] They usually require orthopedic treatment, orthognathic surgery, and fixed orthodontics, often combined to achieve maxillary protraction or mandibular retraction.[4] Moreover, a multidisciplinary treatment approach that includes restorative or prosthodontic treatment may be implemented when replacement of missing teeth is also required, either with simple removable or fixed prosthesis, with implant bone augmentation procedures, depending on case esthetic or functional needs.[4-8]
CASE REPORT
A 45-year-old woman with skeletal class-3 malocclusion presented, wishing to replace her old broken upper acrylic removable partial denture (RPDs). She wore the denture for 10 years, and it recently fractured during lunch. Her medical history was not relevant and her dental history disclosed that she visited the dentist regularly and had done previous fillings and extractions. She was a non-smoker and presented with excellent oral hygiene, brushing and flossing her teeth twice daily. On extra-oral clinical examination, class-3 skeletal profile was noted with the retrognathic maxilla and prognathic mandible, also evident when she wore her old denture. On temporomandibular joint examination, no abnormal signs or symptoms were noted. Maximum mouth opening was 4 cm. Smile assessment revealed a low lip line [Figure 1].

- Pre-treatment extra-oral photos. (a) Frontal view. (b) Smiling view. (c) Lateral view, (showing insufficient lip support and concave profile). (d) Old broken denture. (e) Smiling view with the patient wearing the denture showing poor smile esthetics due to the presence of anterior cross-bite and wide buccal corridors. (f) Lateral view with the denture, showing concave skeletal class-3 profile.
On intra-oral examination, heavily restored dentition could be seen, with fillings on most of her, 14 remaining teeth and 17 teeth were missing. On periodontal examination, there was no bleeding on probing or plaque present on her teeth. The static occlusal examination revealed a class-3 canine relationship and no molar relationship due to missing first molars. She had a negative overjet of 8 mm and no overbite relationship present, with 1 mm shift of the lower teeth to the left from the facial midline. During lateral excursions, she had canine guidance on the left side and group function on the right, with no interferences present [Figure 2].

- Intra-oral views, showing anterior cross-bite and reverse overjet. (a) Right lateral view. (b) Frontal view. (c) Left lateral view. (d) Upper occlusal view. (e) Lower occlusal view.
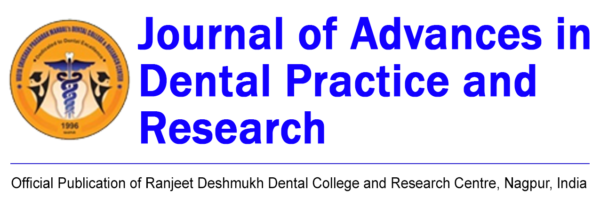
- Pre-treatment radiograph. Orthopantomogram showing 17 missing teeth and resorbed upper and lower edentulous ridges. 27 Over-erupted.
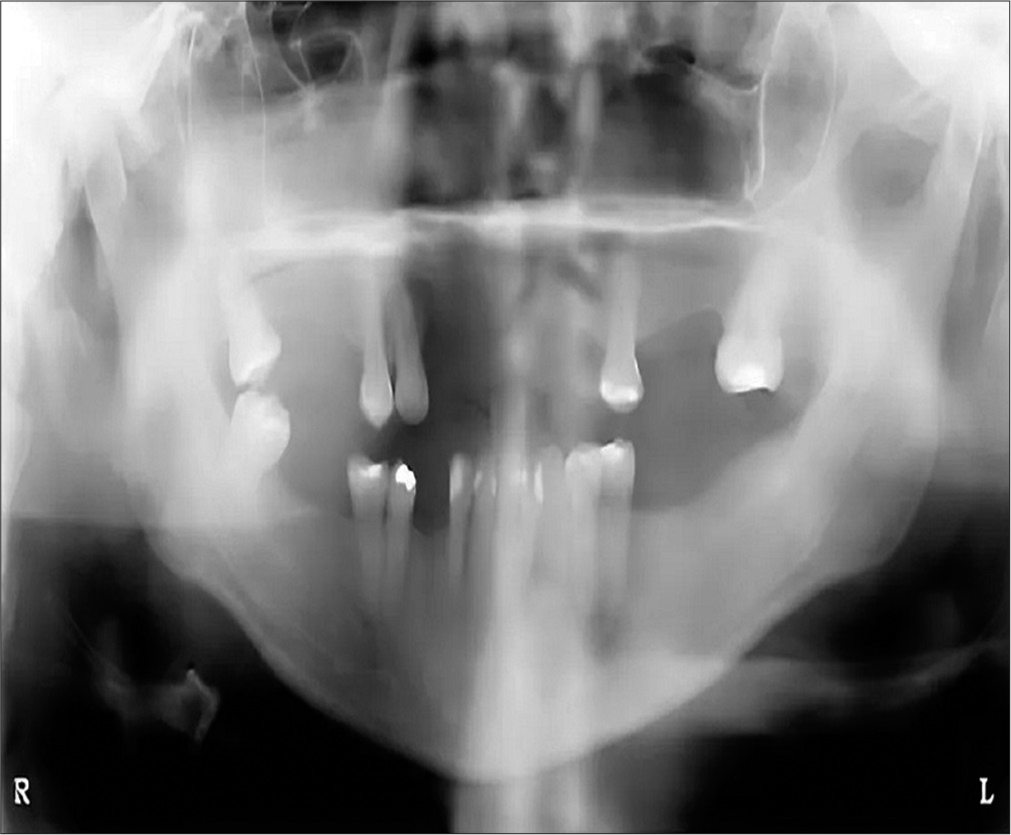
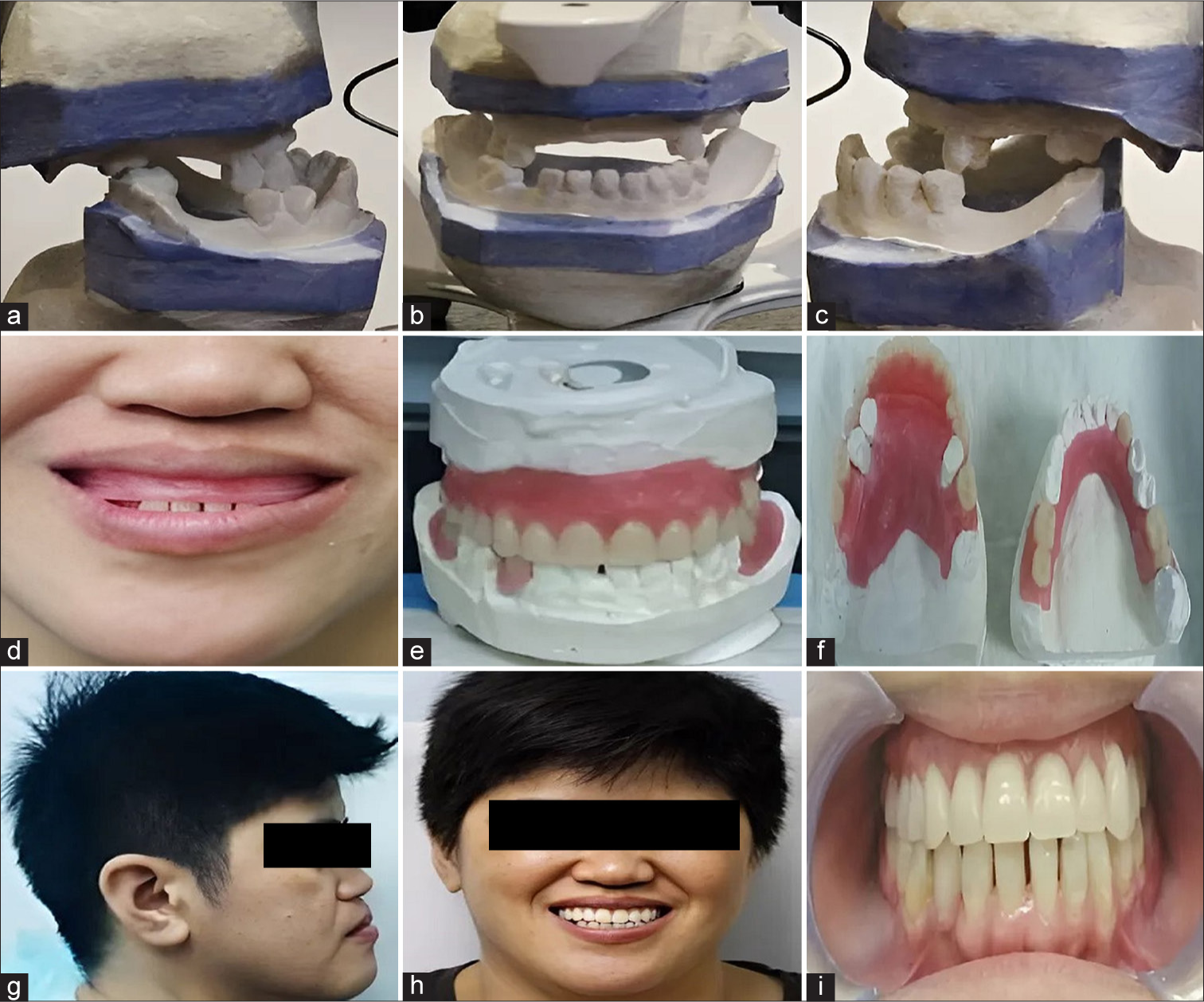
On protrusive movements, the anterior guidance was on premolars and molars. The freeway space was 2 mm. On clinical examination of her prosthesis, the upper denture was in anterior lingual cross-bite, loose with fractured clasps, incisal edge of 12 was fractured. The acrylic teeth shade was darker than her natural teeth. Excellent denture hygiene was noted [Figure 1]. On radiological examination, using orthopantomogram, over-eruption of 27 was noted, with marked resorption of maxillary ridge anteriorly and mandibular ridges posteriorly [Figure 3]. Diagnostic casts were fabricated for further occlusal examination [Figure 4]. The Kennedy classification for the upper arch was class-3 modification-2 and for lower arch was class-2-modification-2. On the basis of the combined above clinical and radiographic examinations, the diagnosis was skeletal class-3 malocclusion, with negative overjet of 8 mm, with partially edentulous upper and lower ridge. She was presented in detail with all alternative treatment options for the replacement of her missing teeth. However, she wanted new RPDs. Therefore, the treatment objective was to construct a definitive cast RPDs that would establish a class-1 jaw relationship and hence provide her with improved esthetics, occlusion, mastication, and speech. The treatment plan included the construction of provisional acrylic (RPD) for initial assessment, followed by the definitive cast (RPD) over 7 month’s period. The treatment plan started with scaling and polishing of her teeth and she was educated on the prevention of caries and periodontal disease. Next, the fabrication of provisional acrylic (RPD) was planned using diagnostic study casts, which was used to design the diagnostic wax-up. Wax-up with acrylic teeth setup was fabricated for initial assessment of lip support, occlusion, speech, and esthetics. Overlay cast (RPD) was planned for the upper arch and cast (RPD) for the lower arch [Figure 4]. To achieve class-1 occlusion and maximum esthetics, it was necessary to replace the maxillary ridge and lip deficiency with an increased flange thickness of 10 mm. It included overlay denture design that enveloped and camouflaged the maxillary canine and premolars within the denture framework, ensuring that there were no interferences during anterior or lateral excursions or functional interference. The occlusal scheme planned was anterior incisal guidance and canine guidance or group function in lateral excursions. The vertical dimension of occlusion (VDO) was increased by 5 mm, which causes the mandible to move downward and backward, increasing overjet and space for restorative adhesive materials.[2] After wax-up approval, a provisional (RPD) was constructed, copying the same denture design. Retention in the upper denture was obtained mainly from favorable teeth undercuts surrounding the upper canine, premolars, and molars obtained after surveying the diagnostic casts. Retention in the lower denture was obtained through wrought wire clasps encircling the lower premolars and molars present on both sides of the mandibular arch. It was used to assess the new lip support, esthetics, new (VDO), speech, and mastication for 3 months period. After 3 months of recall, she was satisfied with the provisional RPDs function and esthetics, copying the dentures design on cast RPD [Figure 5].
- Diagnostic casts and wax-up. (a) Lateral view of diagnostic cast. (b) Frontal view of diagnostic cast. (c) Left lateral view of diagnostic cast. (d) Frontal view showing the maxillary labial flange of the wax up before teeth setup. (e) Frontal view of the wax up. (f) Occlusal view of the wax up showing the planned upper maxillary overlay denture design which camouflages the upper canine and premolars within the overlay denture framework for best esthetics and retention. (g) Patient showing class-1 profile with the wax up noting the improvement after increasing the thickness of the upper labial flange to 10 mm. (h) Improvement in smile esthetics with the designed wax-up. (i) Intra-oral view of the wax-up showing class-1 incisor relationship.

- Provisional removable partial dentures, copied from the wax-up. (a) Frontal extra-oral view. (b) Occlusal extra-oral view. (c) Frontal intra-oral view.
Next, the definitive restorative phase was started. The proximal gaps between her lower anterior teeth were closed with free-hand direct composite restorations buildup as she thought they were unesthetic. Clinical stages of cast (RPD) were then executed in a routine manner. The upper denture design included the palatal plate as the major connector for complete palatal support since <6 teeth were remaining. Further more, direct support for the upper denture was obtained by placing rests mesially and distally on 14, mesially on 17, cingulum rest on 23, mesial and distal rest on 24 and mesial rest on 27. For retention, c-clasp on 17 and 27, palatal clasps on 14 and 24. Lower arch dental design included lingual bar as the major connector cingulum rest on 42, distal rest on 45 and, mesial rest on 44 and 47, and mesial rest on 35. For retention, a rest-proximal plate and I bar was used on 35, c-clasp on 45 and 47. To prevent displacement of the distal extension base of the lower denture, indirect retention of the denture was required, which was facilitated by placing a cingulum rest on 42 and mesial rest on 44. The anterior guidance was copied from provisional RPD using a custom incisal guide table and the same VDO replicated. The final dentures fitted well [Figure 6].
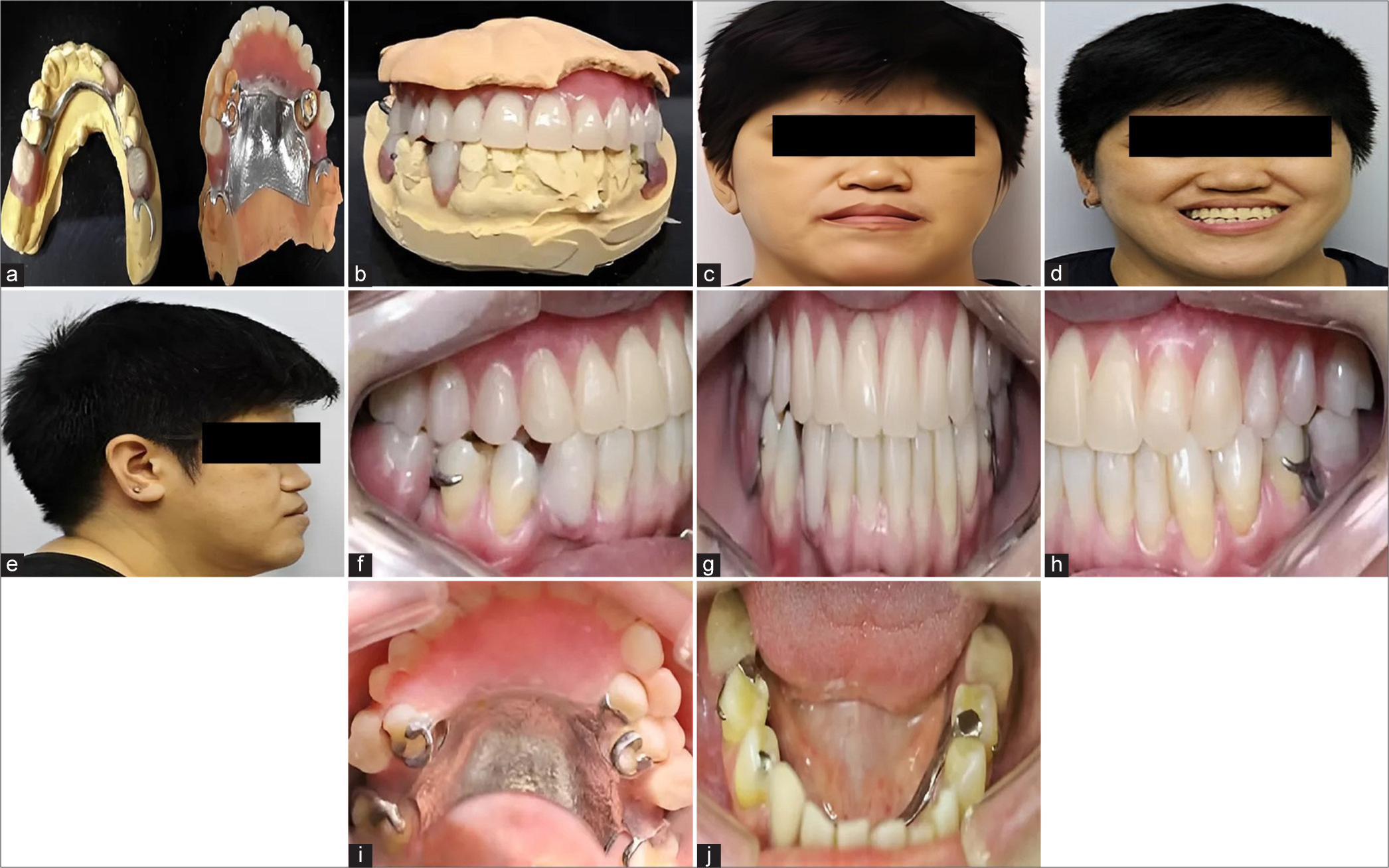
- Final removable cast partial dentures. Provisional partial dentures design was copied into the final cast overlay and removable partial dentures after patient’s satisfaction with the provisional dentures, with regard to function and esthetics. Extra-oral views. (a) Occlusal view of the cast showing the cast partial design. (b) Frontal view of the cast with cast partial dentures. (c) Frontal view after wearing the cast partial denture. (d) Smiling view with the denture. (e) Lateral profile view with the denture. Intra-oral views. (f) Right lateral view. (g) Frontal view. (h) Left lateral view. (i) Upper occlusal view. (j) Lower occlusal view.
DISCUSSION
In the present case, RPDs were considered the most appropriate treatment option, primarily due to patient’s request, the possibility of esthetic replacement of the large upper alveolar ridge deficiency with labial flange, her long 10 years history of successfully wearing RPDs, with demonstration of excellent oral and denture hygiene. With careful surveying, suitable abutments, soft tissue and teeth undercuts were identified and used to determine clasp design and path of insertion, overcoming common problems with RPDs, for example, unattractive metal clasps, retention, and stability.[9]
Treatment drawbacks, for example, development of caries and periodontal disease with poor oral hygiene, or mechanical complications, for example, clasp fracture, debonding, and discoloration of the dentures or composite restorations, and their periodic maintenance requirements were also clearly emphasized to her.[10] After 2 year’s review, abutment teeth had sound pulpal and periodontal health, no signs of occlusal wear or fracture of composite restorations or RPDs were observed. The treatment objectives were successfully achieved and excellent esthetic and functional result was obtained.
CONCLUSION
Removable partial or overlay dentures are minimally invasive, low-cost, and time-efficient prosthodontic treatment options of partially edentulous patients with skeletal class-3 malocclusions when orthodontic, orthognathic, or implant with bone augmentation surgeries are not feasible in which the key factors to success of the treatment relies on: good case selection with treatment planning and selection of the ideal restorative prosthesis and materials.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Skeletal class III malocclusion treatment using mandibular and maxillary skeletal anchorage and intermaxillary elastics: A case report. Dental Press J Orthod. 2019;5:52-9.
- [CrossRef] [PubMed] [Google Scholar]
- Prosthodontic treatment of an angle III class malocclusion: A case report. Quintessence Int. 2017;20:625-31.
- [Google Scholar]
- Prosthetic rehabilitation of the class 3 malocclusion: A case report. Indian J Med Res. 2022;11:24-8.
- [CrossRef] [Google Scholar]
- Combined orthognathic surgery and prosthetic treatment for class III skeletal malocclusion. Stomatos. 2013;19:9-19.
- [Google Scholar]
- Clinical showcase--Correction of an anterior crossbite with a fixed partial denture. J Can Dent Assoc. 2008;9:791-4.
- [Google Scholar]
- Contemporary implant dentistry (3rd ed). United States: Indiana University, Mosby Elsevier; 2008. p. :383-7.
- [Google Scholar]
- Overdenture prosthesis: Alternative to orthodontic and orthognathic surgery: A case report. Balkan J Stomatol. 2011;15:109-12.
- [Google Scholar]
- Alternative esthetic and cost-effective therapy using a removable partial overdenture for the treatment of a patient with class III malocclusion. Braz J Oral Sci. 2006;16:985-90.
- [Google Scholar]
- Oral diagnosis and treatment planning: Part 7. Treatment planning for missing teeth. Br Dent J. 2012;213:341-51.
- [CrossRef] [PubMed] [Google Scholar]
- Maxillary and Mandibular overlay removable partial dentures for the treatment of posterior open-occlusal relationship: A clinical report. J Prosthet Dent. 2002;87:587-92.
- [CrossRef] [PubMed] [Google Scholar]