Translate this page into:
Treatment of non-compliant skeletal class II malocclusion with a hybrid appliance – A case report and review literature
*Corresponding author: Laishram Bijaya Devi, Department of Orthodontics and Dentofacial Orthopedics, Dental College, Regional Institute of Medical Sciences, Imphal, Manipur, India. drbijaya_23@yahoo.in
-
Received: ,
Accepted: ,
How to cite this article: Devi LB, Murmu DC, Lepcha PT. Treatment of non-compliant skeletal class II malocclusion with a hybrid appliance – A case report and review literature. J Adv Dental Pract Res. 2024;3:22-6. doi: 10.25259/JADPR_16_2024
Abstract
The present case describes a case of skeletal deep bite class II malocclusion treated efficiently using the Forsus appliance, and its importance of clinical and biomechanical considerations. Skeletal deep bite class II malocclusions with deficient mandibles are treated with different functional appliances. There are several appliances for its correction in a growing child. However, fixed functional appliances are commonly used in the present clinical scenario for those non-compliant cases, who present late with less residual growth or no growth. This case was treated with a pre-adjusted edgewise appliance supplemented with a device known as Forsus Fatigue Resistant Device (FFRD) (3M Unitek Corp, California, USA). FFRD is a good alternative device for skeletal deep bite class II malocclusions instead of class II elastics in mild cases and place of Herbst appliance in severe cases. Biomechanical principles should be considered for those patients with the Forsus appliance to prevent complications. There are fewer complaints from the patients and treatment time is less.
Keywords
Biomechanism
Forsus appliance
Pre-adjusted edgewise appliance
Skeletal deep bite
INTRODUCTION
Class II malocclusion counts approximately 15% of all malocclusions. It is a state in which the permanent lower first molars occlude distal to the normal relationship with the upper first molars. It has sub-typed into dental and skeletal. The dental sub-type is characterized by a normal skeletal maxilla-mandibular relationship associated with the dental class II molar relationship. Those class II molar relationships with skeletal discrepancies and retrognathic mandibles relative to other craniofacial structures are described as class II skeletal deep bite malocclusions.[1-3]
Fixed functional appliances (FFAs) may also be termed as intermaxillary non-compliance class II correctors, which again can be classified as rigid (e.g., Herbst appliance), flexible (e.g., Jasper jumper), and hybrid (e.g., Forsus fatigue resistant device [FFRD]). These hybrid forms are a combination of flexible and rigid force systems and they are structured to be used continuously for mandibular growth stimulus and are more patient-friendly due to their smaller size and better adaptation to oral functions.[1-3]
The Forsus appliance is a semirigid and hybrid type of FFA used most frequently for treating Class II malocclusions. This appliance is used for patients with less pubertal growth spurt or after puberty.[4-8]
Forsus is also considered an interarch push spring which is a mixture of optimum strength and flexibility and has a spring and a rod with push force. The spring attaches to the distal of the upper first molar while the rod can be placed either distal to the cuspid or 1st pre-molar bracket. This pushing force produces about 200 g of force when fully pressed which makes a forward movement of the mandible.[9,10]
Even though there are works of literature on complications encountered during FFRD therapy, the efficiency and patient-friendly nature is acceptable. At the same time, the patients should be cleared about the knowledge of complications, including flaring of lower anterior teeth and safety measures to have good results.[11-13]
This case presents the clinical efficacy of FFRD and its biomechanical considerations for the treatment of skeletal class II malocclusions at the age of 13 years who reported the chief complaint of forwardly placed upper front teeth.
CASE REPORT
A 13-year-old female patient reported a chief complaint of forwardly placed upper front teeth. There were no significant medical and dental histories.
Extraoral examination
It revealed a symmetric and mesoprosopic facial type and mesocephalic head form. The soft tissue profile indicated a convex profile with positive virtual treatment objective (VTO), and the lips were incompetent with an interlabial gap of 7 mm and a lower lip trap [Figure 1].

- Pre-treatment extra-oral and intra-oral photographs.
Intraoral examination
She had proclined upper anterior teeth with a large overjet of 10 mm and a deep and complete overbite of 6 mm. She had a class II incisor and canine relationship and Angle’s class II endon molar relationship and ovoid-shaped arches [Figure 1].
Radiographic assessment and analysis
The panoramic radiograph demonstrated fully developed permanent dentition with developing wisdom teeth with adequate bone support for all the quadrants [Figure 2]. Lateral cephalogram showed cervical vertebrae maturation indices (CVMI)-Stage IV. The findings showed a skeletal deep bite Class II pattern with ANB of 6° [Figure 2 and Table 1].

- Pre-treatment orthopantomogram and lateral cephalogram.
| Parameters | Pre-treatment | Post-treatment |
|---|---|---|
| SNA (82°±2°) | 84° | 82° |
| SNB (80°±2°) | 78° | 80° |
| ANB (2°) | 6° | 3° |
| Wits appraisal (0–1 mm) | 3 mm | 1 mm |
| FMA (25°) | 27° | 26° |
| SN-MP (32°±2°) | 29° | 28° |
| Y-axis (59°±3°) | 58° | 56° |
| Bjork’s sum (396°±6°) | 398° | 393° |
| Jarabak ratio (62–65%) | 58% | 58% |
| Upper anterior facial height (45%) |
48% | 45.5% |
| Lower anterior facial height (55%) |
52% | 54% |
| Maxillo – Mandibular difference |
20 mm | 22 mm |
| IMPA (90o) | 96° | 98° |
| Max 1–NA (22°±4°; 4mm) | 28°; 7 mm | 24°; 4 mm |
| Mand 1–NB (25°±4°; 4 mm) |
18°; 3 mm | 24°; 5 mm |
| Interincisal angle (131°±2°)) |
123° | 125° |
| Nasolabial angle (102°±8°) | 96o | 108° |
| Upper lip–E line (−4±2 mm) |
−1 mm | −2 mm |
| Lower lip–E line (−2±2 mm) |
−3 mm | −1 mm |
| Overjet (2–4 mm) | 10 mm | 3 mm |
| Overbite (2–4 mm) | 6 mm | 2 mm |
SNA: Angle between Sella/nasion plane and Nasion/point A plane, SNB: Angle between Sella/nasion plane and Nasion/point B plane, ANB: Angle between Point A/nasion plane and Nasion/point B plane, FMA: Frankfort-mandibular plane angle, SN-MP: Angle between Sella/nasion plane and mandibular plane, IMPA: Angle between lower incisor long axis and mandibular plane, NA: Nasion point A plane, NB: Nasion point B plane, E-line : Ricketts esthetic plane
Diagnosis
The patient was diagnosed with skeletal deep bite Class II jaw relationship with Angle’s Class II division 1 malocclusion.
Treatment objectives
Treatment objectives were the correction of class II relationships, proclination, overjet and overbite, and facial profile improvement.
Treatment plan
Treatment involved non-extraction fixed mechanotherapy using a pre-adjusted edgewise appliance (MBT prescription - 0.022 slot) to level and align both arches followed by mandibular advancement using FFRD.
Treatment progress
Initial leveling and aligning were done using 0.016” Nickel Titanium arch-wires followed by 0.016 × 0.022” and 0.019 × 0.025” Nickel Titanium wires. After initial leveling for 4 months, 0.019 × 0.025” stainless steel wires were placed with labial root torque in the lower wire. Then, FFRD (3M Unitek Corp, California, USA) was installed to position the mandible forward and restrict the growth of the maxilla, which reduced the convexity of the facial profile and helped to achieve a class I relation of the molars and the canines bilaterally [Figure 3]. The FFRD was used for 6 months. Crimps were placed for the activation of the Forsus appliance once a month for the duration of these 6 months. Then, the Forsus appliance was removed and class II elastics (light force) were used for retention for 1 month, followed by settling of occlusion for another month. A fixed appliance was debonded and retainers were given.

- Mid-treatment intraoral photographs with Forsus fatigue-resistant device.
Treatment results
Cephalometric findings showed decreased ANB (2°) with a mild decrease in the SNA angle (82°) and an increase in the SNB angle (80°) resulting in forward positioning of the mandible and soft tissue profile improvement. Angle’s class I molar relationship was achieved and the vertical overlapping was reduced from 6 mm to 2 mm and horizontal overlapping from 10 mm to 3 mm. Removable retainers were delivered. An observation period of 1 year was considered after debonding [Figures 4 and 5, Table 1].

- Post-treatment extra-oral and intra-oral photographs.
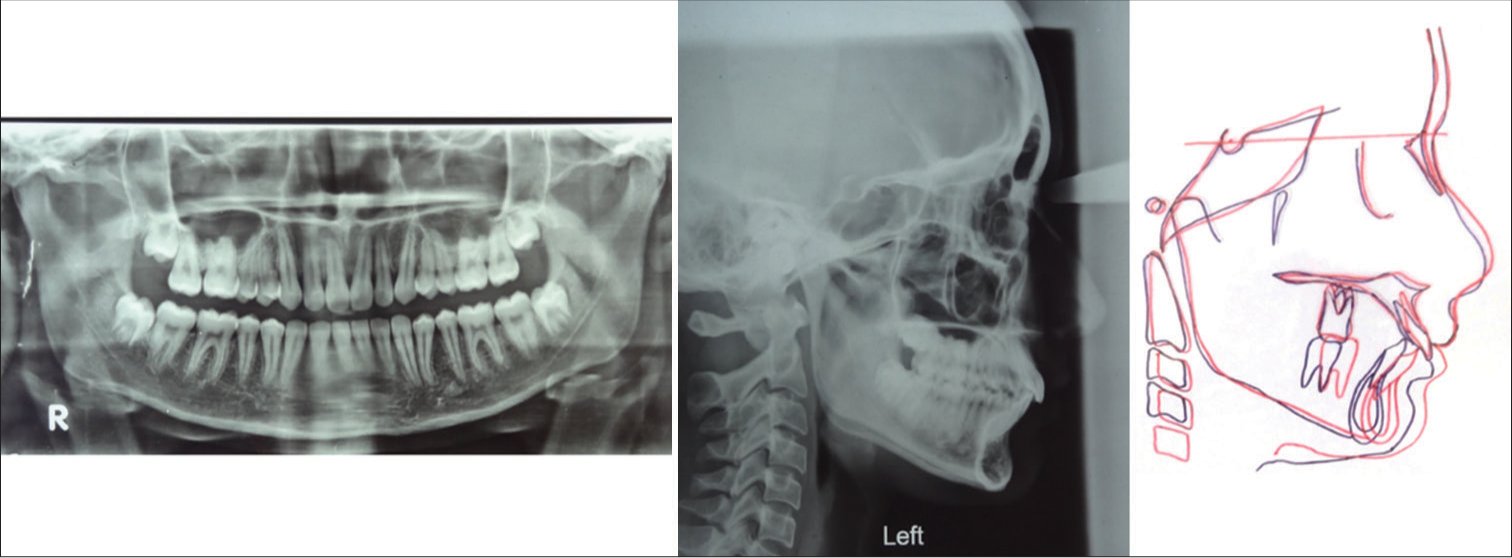
- Post-treatment orthopantomogram, lateral cephalogram, and superimposition, pre-treatment (black lines), post-treatment (red lines)
Biomechanical considerations
Before applying Forsus, initial leveling and aligning is an important phase of the whole treatment procedure. Bonding of the upper second molar is better done along with bonding of the fixed appliance. A continuous rigid archwire (0.019 × 0.025 stainless steel) prevents crown tipping distally and unwanted first molar intrusion. Complete consolidation of the upper arch up to the second molar is necessary to minimize distalization of molars using 0.010” stainless steel ligature wire, which will also help to attain distalization of the whole arch. Adequate bend backs in the lower arch and figure of 8 also helps to prevent flaring of lower anterior teeth. A total of 10° labial torque of the root is given in the lower cuspid to cuspid segment which minimizes tipping in the lower anterior teeth.
DISCUSSION
Class II division 1 malocclusion is a common malocclusion among the Indian population. Either prognathism of the maxilla or retrognathism of the mandible results in this type of malocclusion. In the non-growing cases with mandibular deficiency, camouflage or surgery are the treatment options. [6,10] But for growing individuals, functional appliances are used for growth modification. Exceptionally for those non-compliant patients with less or no residual growth left, FFAs are being used.[7] These functional appliances are given especially when there is a positive visual treatment objective (VTO) with convex profile and no or very mild spacing and very mild crowding permanent dentition. FFRD is a patient-friendly and common device.[8-10]
In the present case, SNA decreased by 2° and SNB increased by 2° showing forward repositioning of the mandible and high-pull headgear-like effect in the maxilla along with dental correction due to distalization of the maxillary arch and partial proclination of lower incisors with labial root torque. It happened successfully due to the residual growth left in the patient.[10]
In the present case, the maxillary incisor to nasion point A reduced from 7 mm/28° to 4 mm/24° while the mandibular incisor to nasion point B increased from 3 mm/18° to 5 mm/24° due to the proclination effect of FFRD on mandibular incisors. Even with an adequate bend back of archwire and figure of 8 were done, the effect of FFRD on mandibular anterior teeth could not be eliminated.[6,10] According to some authors, this proclination effect may be eliminated using mini-screws, larger dimension archwire with labial root torque.[14] With the correction of the molar relation from class II to class I, overjet was reduced from 10 mm to 3 mm and overbite from 6 mm to 2 mm. The class I canine relation was also achieved.
The soft tissue profile improved and became normal and straight from the convex profile and achieved lip competency. There was an increase in nasolabial angle from 96° to 108° and upper and lower lips’ relation to the esthetic line improved from −1 mm to −2 mm for the upper lip and from −3 mm to −1 mm for the lower lip.
Therefore, the use of fixed functional therapy with fixed appliances helped to avoid complicated orthognathic surgery with lesser treatment duration in non-compliant skeletal deep bite class II malocclusion in patients with the presence of residual growth.
CONCLUSION
FFRD is a useful supplement for the management of moderate skeletal deep bite class II malocclusion with fixed appliance. It may also be used as an alternative to elastics in mild cases and Herbst appliances in severe cases. The incorporation of 10° torque in the lower archwire prevents flaring of lower anterior teeth. Incorporation of the trans-palatal archwire and bonding of 2nd molar will also prevent unwanted intrusion of maxillary molars. Correct way of Forsus installation will also significantly improve patient compliance. Clinical and biomechanical considerations discussed in this case report should be given importance for any treatment of skeletal deep bite class II malocclusion with FFRD. These will help to improve patient cooperation and accuracy of treatment duration.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Treatment of skeletal problems in children In: Contemporary orthodontics (4th ed). St Louis: Elsevier Mosby; 2007. p. :495-6.
- [Google Scholar]
- Functional appliances In: Textbook of orthodontics. India: Reed Elsevier Pvt Ltd; 2015. p. :544-45.
- [Google Scholar]
- Interception and treatment of mandibular retrusion with non-compliant fixed functional appliances In: Orthodontics: Diagnosis and management of malocclusion and dentofacial deformities (3rd ed). India: Elsevier; 2019. p. :2717-25.
- [Google Scholar]
- Components of class II malocclusion in children 8-10 years of age. Angle Orthod. 1981;51:177-202.
- [Google Scholar]
- An assessment of late fixed functional treatment and the stability of Forsus appliance effects. Aust Orthod J. 2014;30:2-10.
- [CrossRef] [Google Scholar]
- Treatment of class II division 2 malocclusion using the forsus fatigue resistance device and 5-year follow-up. Case Rep Dent. 2016;2016:3168312.
- [CrossRef] [PubMed] [Google Scholar]
- Use of Forsus fatigue-resistant device in a patient with Class I malocclusion and mandibular incisor agenesis. Am J Orthod Dentofacial Orthop. 2014;145:817-26.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical and clinical considerations in correcting skeletal class II malocclusion with forsusTM. J Contemp Dent Pract. 2012;13:918-24.
- [CrossRef] [PubMed] [Google Scholar]
- Non-extraction treatment of a skeletal class II malocclusion using 'forsus' appliance-a case report. J Dent Med Sci. 2019;18:74-80.
- [Google Scholar]
- Treatment of division II malocclusion in young adult with Forsus™ fatigue-resistant device. Indian J Dent Res. 2012;23:288-91.
- [CrossRef] [PubMed] [Google Scholar]
- Complications encountered during Forsus Fatigue resistant device therapy. Dental Press J Orthod. 2020;25:65-72.
- [CrossRef] [PubMed] [Google Scholar]
- Twenty-year clinical experience with fixed functional appliances. Dental Press J Orthod. 2018;23:87-109.
- [CrossRef] [PubMed] [Google Scholar]
- Functional and social discomfort during orthodontic treatment--effects on compliance and prediction of patients' adaptation by personality variables. Eur J Orthod. 2000;22:307-15.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment effects of the Forsus Fatigue resistant device used with miniscrew anchorage. Angle Orthod. 2014;84:76-87.
- [CrossRef] [PubMed] [Google Scholar]